Taking a piece of subcutaneous fat from a sacrificed mouse and implanting in to the mesentery of a recipient mouse causes weight loss in the recipient, starting once the surgery has healed. We know that healing takes something just over six weeks:
Is the effect replicable? Yes, fairly well, here it is in a second cohort by the same group:
While this is pretty certain, the explanation is very speculative. Note the effect kicked in slightly sooner in cohort 2, I would assume that healing was a little quicker for this cohort. Maybe the researchers got better at performing the surgery. The 12 week weights are essentially identical between cohorts.
So......... Adding extra adipocytes causes overall fat loss, as in this image from Cohort 1 featured in the last post:
I find this rather interesting, to say the least. The black squares represent mice which have had subcutaneous adipose tissue implanted around their mesentery so that a significant proportion of its venous drainage enters the portal vein and goes directly to the liver.
I've looked through the data from the paper for any suggestion as to an explanation of why the weight loss occurred. There is nothing anywhere to suggest uncoupling while the mice where in the CLAMS apparatus (though calorie restriction is a good way to suppress uncoupling acutely). Calorie malabsorption through surgical damage to the mesentery seems unlikely as similar surgery to implant visceral fat gave normal weight gain compared to control mice.
So I think the mice in the SC-VIS group simply cut their ad-lib calories. Food intake was only measured over the one day in the CLAMS apparatus so we'll never know what the overall food intake was relative to controls, but I can't see any other explanation.
Which leads to the question as to why they might have cut calories, other than the obvious: They we not as hungry as the control mice. This effect occurred with mesenteric implanted subcutaneous adipocytes, but not with implanted visceral adipocytes. So we have to ask what the difference might be between the adipocyte types.
Visceral adipocytes are more insulin sensitive than subcutaneous adipocytes. They will store fat more easily and refuse to release it until insulin drops down to absolutely basal levels. On an ad-lib high carbohydrate diet this will not happen very often. As far as the liver is concerned, the visceral fat in the mesentery and omentum is non existent for most of the time. Adding extra visceral adipocytes at this site will not change this.
Subcutaneous adipocytes are less sensitive to insulin, they will store fat at high insulin levels but release FFAs easily as insulin levels fall. Obviously, they are always smaller than visceral adipocytes and they stay that way when implanted in to the recipient mice. If they are implanted in a location from which their easily released FFAs go directly to the liver they are in a position to have a metabolic effect.
Summary of the speculation so far: Visceral fat adds nothing to the FFA level of portal vein blood unless insulin level is well below that of a mouse on ad lib standard mouse chow. Placing subcutaneous adipocytes where their venous drainage goes directly to the liver supplies supplementary FFAs directly to the liver when insulin levels are merely low rather than rock bottom.
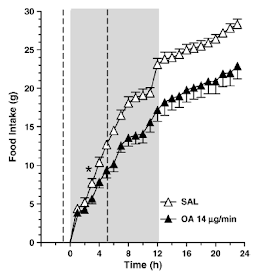
It has been known for a very, very long time that infusing FFAs in to the portal vein suppresses appetite and that this effect requires a functional vagal nerve supply to the liver. This group of rats is receiving an oleic acid infusion (if you are going to secure a long term cannula in to the portal vein then something larger than a mouse might make the surgery slightly more practical and less challenging) in to their portal vein:
Hepatic-portal oleic acid inhibits feeding more potently than hepatic-portal caprylic acid in rats
Oleic acid infused in to the portal vein at 14mcg/min for six hours reduced food intake during the 12 hour dark period from 23g in the controls to 17g in the oleic acid group. At 14mcg/min the infusion supplies 840mcg/h and over six hours this supplies just over 5mg, ie 0.005g in total dose, roughly 0.05kcal, 0.21kJ of oleic acid. This is enough to drop food intake by six grams of food at 12.4kJ/g, ie 74kJ.
This group looked at 14mcg/min because they knew it would work. We don't know how low an infusion rate could go while still having an effect on appetite (from this paper anyway). The two unanswerable questions we are left with are: What was the augmentation of FFA supply to the liver from SC adipocytes in the mesentery of the operated rats in Kahn's study? Was this enough to limit food intake? We don't know the answers but you can imagine what my guess is.
Getting access to the portal vein to either measure or infuse anything is a complete surgical nightmare. Kahn's group looked at all sorts of systemic messengers in terms of cytokines and adipokines and found absolutely nothing to explain their phenomenon.
Perhaps they were looking in the wrong place.
Peter
I guess the third question is why the SC adipocyte recipient mice actually ate a little more than the controls in the CLAMS apparatus (as judged by RQ). I'd still bet on differences in total fat mass available over-riding the stress induced refusal to eat, irrespective of degree of hunger in any mouse through the rest of the study... You could throw in cortisol, adrenalin and the lack of neural innervation of transplanted adipoctes but let's leave it simple (and possibly incorrect).
More supplementary speculation: Is the normal profound fall in appetite on induction of ketogenic eating in humans directly related to the sudden access to visceral abdominal fat, secondary to the major reduction in circulating insulin? This would suggest that the satiating effect of ketogenic diets might be more marked in people with significant visceral obesity. It would become less obvious as weight loss progresses until the majority of remaining fat is where it should be, in the non-visceral adipocytes of a normal shaped human being... The effect might even be virtually non existent in young, fit, healthy folks who would simply eat under ketosis to maintain their current rather normal bodyweight.



The first two comments on this post are spam. Here's hoping they are dealt with anon.
ReplyDeletePeter, I got a little confused in the last few paragraphs. I thought all the fat transplantation experiments were performed on mice? Not rats?
"What was the augmentation of FFA supply to the liver from SC adipocytes in the mesentery of the operated rats in Kahn's study?"
"I guess the third question is why the SC adipocyte recipient rats actually ate a little more than the controls in the CLAMS apparatus..."
Thanks cave, any other transpositions spotted would be gratefully received!
ReplyDeletePeter
Interesting
ReplyDeleteIt seems adding SQ fat whether SQ or visceral lowered wt, whereas SQ fat located messenteric was most effective to reduce wt. Its noted in rodents higher leptin causes linear and progressive wt loss, so i would assume the body wt reducing effects of higher adipocytes in rodents to mostly be a leptin thing, with an additional benefit of transplant close to portal circulation to enhance effect.
Even though a hypothesis can be made adipocytes are dumping FFA producing satiety we also must account that insulin concentrations are higher near portal circulation, so subcutaneous adipocytes transplanted here will have more lipolysis suppression than if they were conventionally planted more peripherally. So, though subq adipocytes are more IR, they will be *less* lipolytic if transplanted to an area of the body with a higher insulin concentration. In other words SQ fat peripherally would be less antilipolytic, than SQ fat near portal circulation, due to a higher exposure to insulin.
Another possible interpretation is perhaps increasing adipocytes so close to the liver may have a triglyceride lowering effect, an intervention which is noted to produce leptin supersensitivity. Extra normal adipocytes themselves will contribute to elevated leptin levels, combined with adding adipocytes with more insulin stimulation near portal circulation to better attenuate leptin-resistance promoting triglyceride excess. Its too bad serum triglycerides were not measured.
Higher leptin level (more normal sized adipocytes) + lower triglycerides -> wt loss.
It could as well just be an effect of higher leptin alone; assuming these were normal adipocytes, the level of leptin should increase, as would total body fat. Wt loss then occurs, consistent with leptin treatment of rodents.
In humans who are normal increasing leptin does not really induce wt loss so i would expect SQ transfers in humans to just increase fat mass, although SQ in mesentery may correct dyslipidemia of TG excess that prevents BBB leptin transport, as it likely did in these rodents.
One more thing, SQ adipocytes close to portal circulation will also be exposed to more insulin attenuating lipolysis, but more importantly, provoke exaggerated leptin synthesis.
ReplyDeleteI think FFA is unlikely to be mechanism as the rodents had superior glucose tolerance and reduced hepatic glucose output, which usually would not occur if there was a greater shift to fat metabolism, but it is highly consistent with a leptin effect as leptin is enormous in regulating hepatic glucose output. Leptin treatment alone can controlt ype 1 diabetes which is largely mediated by disinhibited glucagon. But this is expected if SQ adipocytes in mesentary were making more leptin, particularly right near the liver.
Hi Wooo, As you well know I have a horrible blind spot on leptin. I looked at figure 3A where leptin is very low in the systemic circulation and just thought “Well, they’re skinny…”. We’d be talking implanted adipocyte/liver leptin crosstalk here (?) which is out of my field of reading. I hadn’t considered an increase in exposure to insulin. Obviously the insulin in the HPV is much higher than in the systemic circulation. The question then becomes one of asking where the arterial supply to the transplants arises from (mesenteric artery? i.e. systemic?) so I’m still not sure… I have to admit that I was expecting that the portally released FFAs, if they are real, would induce hepatic insulin resistance but the portal infusion data look to be at much lower rates than the rates supplied by whole body lipolysis under starvation, where hepatic insulin resistance should occur. So if the effect is via portal FFA the effect should require low-but-not-zero supplementation from the SC adipocytes.
ReplyDeleteI also looked at the 14C-DG uptakes in Fig4 but these only show basal vs (what I assume is supra maximal, it’s not in the methods) insulin. Probably tells us nothing except how much “room” is present in a given adipocyte in each population, rather than physiological responses during rising/falling insulin levels. All of the transplanted SC adipocytes stay small, transplanted VIS adipocytes grow very slightly, but they are pretty big to being with.
It’s certainly an interesting paper which opens up all sorts of ideas. I think the authors have a long way to go.
Pete
Somewhat unrelated:
ReplyDeletehttps://www.theguardian.com/society/2018/jun/10/converting-bad-fat-to-good-fat-a-new-means-of-tackling-obesity
How do 50 - 100 g of brown fat, which probably contain less mitochondriae than several kg of muscle or 1.4 kg of brain, manage to burn through 20% of daily calories??