This is a study which Raphi threw out on Twitter several weeks ago. It can take me personally this long to understand some studies. It's interesting as it clearly shows that weight loss over 12 weeks causes a deterioration in insulin sensitivity in some people:
They started with 52 obese people and ended up with 38 who completed this part of the study. On average insulin resistance dropped with weight loss.
On average, that is. It did for some. For others it didn't. Yes, in nine of the group of 38 subjects, insulin sensitivity deteriorated with weight loss. As the authors comment:
"Thus, it may seem paradoxical that some of the changes observed in the present study during weight loss prevented an increase in insulin sensitivity."
"Thus, it may seem paradoxical that some of the changes observed in the present study during weight loss prevented an increase in insulin sensitivity."
I love a paradox.
What is going on?
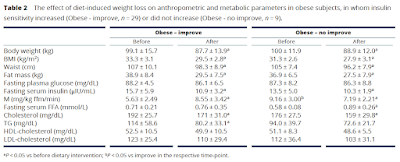
Here are the metrics from Table 2
Here are the metrics from Table 2
The paradox comes from the M values.
These are the clamp values. Insulin was infused to maintain a plasma level of 80microIU/ml and hypoglycaemia was avoided by infusing glucose to maintain a plasma level of 5mmol/l. If you do this for 2h you can assume some sort of steady state is achieved and the M value is the rate of infusion of glucose needed to counteract insulin's hypoglycaemic effect over the final 40 minutes of the clamp. The higher the M value the better insulin is working and the less insulin resistant your subject is. This is the gold standard, HOMA-IR is the poor relative (though much easier to estimate and wouldn't have shown any paradox in this study).
So in nine subjects the M value deteriorated with weight loss.
The subjects were divided on the basis of the direction of this change in M score resulting from weight loss.
To cut a long story short the group which deteriorated their M score were obese but had normal insulin sensitivity before weight loss. The so-called metabolically healthy obese. The subjects whose M score actually improved were insulin resistant before weight loss.
From a previous paper by the same group the M score in a group of lean control subjects (not described here but part of the overall study) was 9.77mg/kg ffm/min and here, for the obese but insulin sensitive group M, it was 9.17mg/kg ffm/min, ie no difference. In the obese but insulin resistant subjects pre weight loss M values averaged 5.63mg/kg ffm/min, ie low, p<0.05.
The first question is: why should metabolically healthy, insulin sensitive obese people deteriorate their insulin sensitivity score as a result of weight loss?
That's the simple one. They're losing weight and have not stopped at the time of the hyperinsulinaemic clamp. Their diet is providing completely inadequate calories to maintain stable weight so they are losing some weight, mostly from fat. The process of weight loss involves releasing FFAs from adipocytes with an associated rise in plasma FFAs and subsequent oxidation of those FFAs. I did a ball park rough calculation and someone of my height (but obese) would have been on 1400kcal per day, ie they would be hungry and oxidising body fat to make it up to the well over over 2000kcal I'm considered to require to run my metabolism.
Aside: Obviously from the Protons perspective oxidising fatty acids will generate ROS irrespective of mitochondrial delta psi and the cell will resist insulin's signal in proportion to this fatty acid oxidation induced ROS signal. It is apparent that this cannot be suppressed by an hyperinsulinaemic clamp for two hours, see below. End aside.
There is a study which actually measured fat oxidation under an hyperinsulinaemic clamp under conditions of active weight loss. It's this one:
Prolonged Fasting Identifies Skeletal Muscle Mitochondrial Dysfunction as Consequence Rather Than Cause of Human Insulin Resistance
which combines a Dutch version of the M score with indirect calorimetry during the steady state conditions of the clamp. Neat hey? This time weight loss was not from an hypocaloric diet, it was from a zero caloric diet, ie extended fasting, which sources calories from a minimal carbohydrate, minimal protein, very high fat source, ie the subject's own body catabolism. Just for 60 hours. But by the end nearly 100% of calories from are fat oxidation.
Prolonged Fasting Identifies Skeletal Muscle Mitochondrial Dysfunction as Consequence Rather Than Cause of Human Insulin Resistance
which combines a Dutch version of the M score with indirect calorimetry during the steady state conditions of the clamp. Neat hey? This time weight loss was not from an hypocaloric diet, it was from a zero caloric diet, ie extended fasting, which sources calories from a minimal carbohydrate, minimal protein, very high fat source, ie the subject's own body catabolism. Just for 60 hours. But by the end nearly 100% of calories from are fat oxidation.
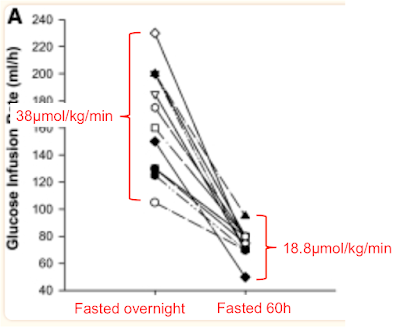
The clamp data come from Fig 2, the rates of disposal of glucose in red come from Table 2 and I've clarified the labels to point out that "Fed" means "Overnight fasted", not post prandial:
The glucose disposal units don't include fat free mass as this doesn't noticeably change in 60 hours of fasting so this means the values can't be directly compared to M values. We can see that glucose disposal halves under hyperinsulinaemic clamp study conditions when 60 hours of fasting necessitates metabolism to be run on fatty acids.
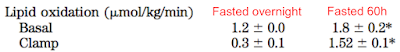
Proof that fatty acid oxidation continues under hyperinsulinamia comes from measurements in a respiratory chamber while the clamp was on-going. From the bottom of Table 2:
After an overnight fast, on a balanced diet, lipid oxidation is 1.2μmol/kg/min and drops to 0.3μmol/kg/min under clamp. During body fat loss for 60 hours the clamp can only suppress lipid oxidation to 1.52μmol/kg/min, ie still higher than under basal conditions before the 60 hour fast. Oxidising lipids intrinsically generates mitochondrial ROS to limit ingress of excess calories by limiting insulin facilitated signalling. Even at clamp levels of insulin exposure.
So weight loss causes insulin resistance because it intrinsically involves fatty acid oxidation. Stopping the weight loss using a period of adequate feeding would allow the weight loss induced insulin resistance to fade away. The only "paradox" is that the changes which occur in the provision and oxidation of fatty acids cannot be immediately reversed by the external application of 80μIU/ml of insulin, at least not within two or three hours.
It's also worth mentioning that this insulin resistance during weight loss is utterly normal and pro-survival from an evolutionary perspective.
Okay. Much more interesting are the patients who do improve their insulin sensitivity with weight loss. Fasting FFAs before weight loss are around 0.71mmol/l, higher than the value of 0.52mmol/l found in the slim control group in the previous section of the study.
This group has metabolic syndrome, ie they do not have the ability to suppress lipolysis using insulin because enough of their adipocytes are "leaking" FFAs via basal lipolysis and so are exposing their peripheral tissues to an on-going supply of FFAs, which are being oxidised continuously whether insulin is present or not. When insulin is present then this unstoppable supply of FFAs necessitates enough resistance to insulin's signal to balance caloric ingress. Glucose disposal under hyperinsulinaemic clamp (M value) stays low at 5.63mg/kg ffm/min because fatty acids are being oxidised, so glucose is significantly excluded. We don't know the FFA concentration under clamp or fatty acid oxidation in this study but my view is this is what is happening.
With weight loss adipocytes shrink. Two things happen. FFA levels rise because weight loss requires fat release. And, as adipocytes shrink, they decrease their size-determined basal lipolysis rate and so restore insulin's ability to suppress FFA release. These opposing factors, in this case, balance out in a trivially raised level of fasting FFAs to 0.76mmol/l, but the release of these FFAs can be suppressed by insulin, so M rises from 5.63mg/kg ffm/min to a respectable 8.55mg/kg ffm/min under the hyperinsulinaemic clamp after weight loss.
Fat oxidation obligates a degree of resistance to insulin's signal to maintain physiological caloric ingress. Protons also suggests some fatty acids do this better than others.
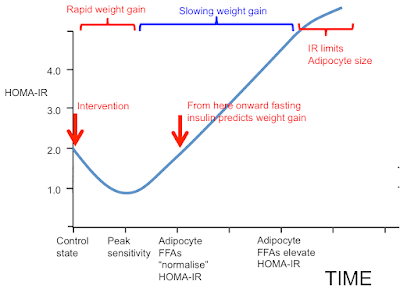
I was going to stop here but I may as well throw this in. People may recall this graph:
Now we can get rid of most of the labelling and insert the concepts discussed in this post. These arrows represent what I consider the situation to be under weight stability, so the situation is not complicated by the level of insulin resistance superimposed by weight loss.
It's easiest to think of the arrows representing the study subjects before 12 weeks on a severely hypocaloric diet. During weight loss the metabolically healthy group will temporarily move their location to the right due to increased fatty acid oxidation resisting insulin. Those with metabolic syndrome will try to do the same but this is offset by shrinking adipocytes decreasing their basal lipolysis so allowing insulin to work and actually improve the M score overall.
I could have stopped here too but I still have a final arrow to add. This comes from Arne Astrup's lab in Denmark. There are no clamp data but under weight stability the M score and HOMA-IR would correlate perfectly well, assuming everyone was on a similar mixed diet. Astrup looked at formerly obese (FO) women who had maintained, through sheer willpower, a normal body weight using conventional dieting. Rare as hen's teeth, but they do exist.
Fat metabolism in formerly obese women
Fat metabolism in formerly obese women
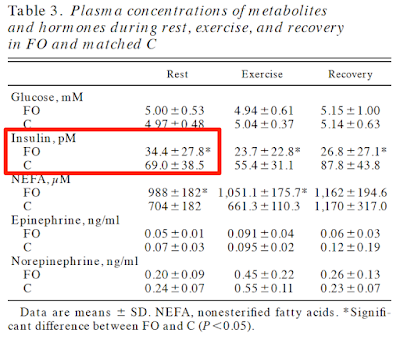
No clamp data but just look at the insulin and glucose values. C is control, FO is formerly obese. Formerly obese ladies are very, very insulin sensitive. Pathologically so:
If we wanted to add these ladies to the graph they would be here, at the blue arrow:
There is a body of opinion on t'internet that holds that insulin resistance causes obesity. They have some explaining to do.
Now I really will call it a day.
Peter




10 comments:
Great, you're back Peter! I must confess I still have to read the whole insulin sensitivity series.
Meanwhile, let me post an only slightly off topic link
Medcram Red Light Therapy Reduces Blood Glucose and Increases Metabolic Rate
https://www.youtube.com/watch?v=6Win49aeh8A
https://www.researchgate.net/publication/373466102_Optical_stimulation_of_mitochondria_reduces_blood_glucose_levels
Very puzzling. Apparently, you get a 27% higher glucose metabolism by exposing an 800 cm² area (a little more than an A4 page of paper) of peoples' back for 15 min with 670 nm light that is either 40 or 17 mW/cm² (paper and reply by author as reported in comment do not agree). The author also reportedly said it worked like a switch, 2 or 20 min didn't make a difference.
The proposed mechanism "670 nm andother, longer wavelengths of red/near infra-red light are absorbed by the nanoscopic interfacial waterlayer surrounding mitochondrial ATP rotor pumps. [7]" strikes me as esoteric to say the least. If true, how does exposing <0.2% of the cells of the body (800 cm² * 2 mm penetration depth) turn up whole body metabolism? If there is really some full body signalling, then the proposed mechanism can't be right.
I was starting to wonder if the entire Hyperlipid community had disappeared into the cosmic oubliette.
Like Eric, I still have to catch up on all the recent insulin sensitivity posts. Just wanted to say I'm glad you're alive and kickin.
Petro - thanks for sharing your analysis.
Very interesting. I have posted in a few places that one HAS to be on the insulin resistant side in order to lose weight. (Thus these ladies that have already lost weight have bodies super sensitive trying hard to gain back that weight - what has perverted the set-point?). The direction of net flux of fatty acids in and out of adipose tissue is dependent on not just the insulin level, but adipose sensitivity. (Remembering that the liver becomes insulin resistant first, muscles second, adipocytes last. ) I think of insulin sensitivity as tissue dependent. In this paper, they are measuring whole body sensitivity(in respect to blood glucose as apposed to measuring FA flux).
Adipose tissue has to be somewhat insulin resistant for the flux of fatty acids to favor weight loss. (it is some function (most likely nonlinear) of sensitivity vs insulin that sets the direction of flux)
The big questions is what causes a shift in the set point that is behind the T2D pandemic? I think it might be more than one thing:
Huge increase in concentrated seed-oil consumption - protons etc
Consumption of artificial sweeteners that trigger receptors down the entire digestive track - increasing insulin.
Antibiotic effect of preservative may well drive some other shift (livestock fed with antibiotics greatly increase weight gain - (I don't think we know much of anything about the mechanism of action of this weight-gain effect. Perhaps a list of how strong an effect vs the type of antibiotic might give a hint?)).
,.,.
Questions:
Are the preservatives triggering receptors in the gut?
Is the cause of T2D set-point perversion a permanent damage - or reversible? (confounded by the long half life of PUFA).
Some antibiotics increase sunburn - and there seems to be a connection with sunburn and Linoleic Acid - do antibiotics mess with the proton ratio?
,.,.
In a sane world, getting to the bottom of T2D (a HUGE cost to society) would be a top priority - but I've come to accept that we have government by the donors; for the donors (technically fascism) - democracy is an illusion. The voice of the people is not heard.
Always good to read whatever pops up here :)))
I am still trying to digest this series. Like most people, well like most insulin resistant tending people like me, I try to work out how this fits my experiences. Having lost something like 40Kilos over the last 15 years but still a little heavy I tentatively put myself on the inital rhs of the low point in that plot. But some things, difficult to relate to. Weight gain = easy, blood sugar tends high, more so if I eat too much fat ( assume fat -> greater insulin resistance ( protons) --- that's logical). Sugar must be coming from gluconeo. But weight gain is sooo easy so must be insulin sensitive so some bit of paradox there, insulin sensitive adipocytes but high blood sugars, sometimes.
I promise not to start this sentence with actually but I had an awful respiratory infection a few months ago, non covid in fact much worse than covid which was no big deal however this infection seems to have thrown a spanner in my blood sugar regulation, only recently is it slowly getting back to where it was. I wonder what it broke, exactly? Seems like a clue.
An apocryphal piece of evidence btw relating to the T1 diabetic kids at one if the schools I work at, the parents often say their kids had some sort of virus or inflammation just before they became diabetic. It could be a chicken and egg situation though in that being diabetic or pre-diabetic can predispose one to infections.
Eric, you may find this interesting, CcO and NO is involved with red light.
https://mct4health.blogspot.com/2023/09/nitric-oxide-tissue-oxygenation-and.html
@Karl " (Remembering that the liver becomes insulin resistant first, muscles second, adipocytes last. ) I think of insulin sensitivity as tissue dependent."
On the face of it this seems like an important aspect. For me trying to make sense of how it works out in practice --- still many paradoxes.
" do antibiotics mess with the proton ratio?"
Medicinal antibiotics are mostly amplified toxins from simpler organisms so the harm potential is increased by several magnitudes of order from what could already be pretty nasty. My intuitions suggest that antibiotics cause huge problems in unexpected places. For instance you'd have to be some sort of ogre to suggest that children not recieve apropriate antibiotics for serious infections but I wonder if the psychotropic effects of them are ignored, nonetheless implicated in several childhood behavioural problems? The cost benefit analysis is tricky and as usual the costs keep getting swept aside in favour of the worthy benefits, until such time as they obviously cause great harm = snafu, the usual medical-industrial way of doing business.
BTW, re semaglutide: Australia’s medicine regulator is investigating several reports of intestinal obstructions in patients using the diabetes turned weight-loss drug Ozempic.
https://www.abc.net.au/news/2023-10-10/australian-drug-regulator-investigates-possible/102958582?utm_campaign=abc_news_web&utm_content=link&utm_medium=content_shared&utm_source=abc_news_web
... orders of magnitude. Duh ..
I wonder how much of an effect the underlying fat content of the diet would have on ethanol-induced insulin resistance?
Oddly, they seem to use olive oil as the fat.
"PPARδ agonist attenuates alcohol-induced hepatic insulin resistance and improves liver injury and repair"
Post a Comment