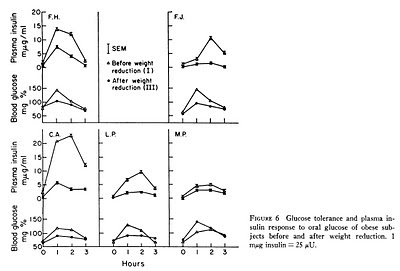
She links to Ruderman's mini review, which we will come back to in some detail in future, and there we find this excellent graph:

I rather like this graph, although it could theoretically be reduced to one line of text. The bit I like best about it is that you can play Pin the Donkey Tail on it. We'll play later.
The graph shows that lipid oxidation, as indicated by respiratory quotient, is well below normal in both pre-obese and post-obese people.
But not in the obese.
No, the RQ of an obese person is, from the graph, somewhere around 0.825, ie an obese person actually runs their whole body metabolism slightly more using fat vs carbohydrate than a non obese person, who has their RQ at around 8.5 when on a mixed diet.
It is only the pre-obese or post-obese who run their metabolism on carbohydrate (poorly) and fail to oxidise fat, their RQ panning out up at 0.875.
If we ignore causes of mitochondrial dysfunction for the time being, we can look at these situations logically. I'm loathe to use analogies but they are useful on occasions. Here's one, highly factual and probably quite relevant:
Take a type 1 diabetic with complete failure to produce any pancreatic insulin. Ask them to volunteer to skip their exogenous insulin, become both profoundly hypoinsulinaemic and markedly hyperglycaemic. Then use a tracer to measure their glucose metabolism. Can they use glucose? Of course they can. This was done back in 1978 and the results are quite clear cut. Acute hypoinsulinaemia can be compensated for by acute hyperglycaemia.
Now, the question is whether there is a situation existing at the mitochondrial surface, as relates to fatty acids, which is analogous to that at the cell membrane surface as regards glucose. Glucose uptake is controlled at the cell surface. Fatty acid uptake is (predominantly) controlled at the mitochondrial surface.
Can we increase intracellular free fatty acid derivatives to the point where energy production can be forced back up to a semblance of normality in the abnormal mitochondria of a pre-obese person?
The graph of RQs suggests to me that this can indeed be done.
However it requires an increase in FFA delivery to the tissues well in excess of what a normal person might oxidise. There needs to be enough of an increase in FFA delivery to the tissues to reach the point where FFA derivatives can be "pushed" down an adequate concentration gradient in to mitochondria to restore adequate ATP production.
The cost of this maneuver is in increased FFA intermediary-derived insulin resistance and even greater failure to use glucose.
If you are having even more problems using glucose because you have managed to get your fat oxidation up by increased lipid derivatives within the cytosol, where would you expect your RQ to be compared to someone who has free choice in metabolic substrate utilisation? More fat, less glucose. So the RQ will be.....
Lower of course. Somewhere around 0.825 I would guess, looking at the graph.
You can see why I like this graph...
So we know that the pre-obese and post-obese have problems burning fatty acids in their mitochondria. We know the currently-obese have corrected this defect by increasing fatty acid delivery to their mitochondria at the cost of worsening insulin resistance.
How do we increase fatty acid delivery to the cytosol? Fatty acid delivery is primarily controlled at the adipocyte level. Insulin, acting on normal adipocytes, inhibits lipolysis. Have I ever said that before?
Adipocyte insulin resistance is the direct equivalent of relative hypoinsulinaemia. If we simply stretch our adipocytes to the point where they no longer listen adequately to insulin we can increase FFAs delivery to the blood stream and so increase their delivery to cytosol and get to work pushing them in to whatever mitochondria we have.
In the state of established obesity energy production is, in fact, normalised.
Let's just set this out:
Mitochondrial dysfunction leads to cytosolic fatty acid derivative accumulation.
This leads to chronic hyperinsulinaemia via insulin resistance.
This leads to adipocyte distension.
This leads to adipocyte insulin resistance.
This leads to increased plasma FFA delivery at a given level of insulin.
This leads to increased cytosolic FFA derivatives.
This leads to mitochondrial ATP production being normalised.
The cost is increased insulin resistance. Oh, and the MECHANISM for improved ATP production is OBESITY. Call this a cost if you wish.
BTW: Of course there is a second set of discussions related to adipocyte mitochondrial dysfunction but I'll leave that out to keep it simple here.
Okaaaaaay.
Time to play Pin the Donkey Tail.
Everybody needs a drawing pin (thumb tack?). And a piece of string attached to it to represent the donkey's tail. It is traditional to have a picture of a tail-less donkey taped to a cork board and to try and pin the tail in the correct place, while blindfolded. I'll let everyone off of the blindfold and we can have this nice blue balloon as a substitute for the picture of the tail-less donkey.
It would be very helpful, if you are doing this at home, to write "Adipostat Hypothesis" on the balloon, most easily done before you inflate it. I couldn't be *rsed to do this, as always.

Now pin the tail, using the thumb tack, on to the balloon.
Pop!
Oops. Did you just pop the set point hypothesis of obesity? Clumsy of you, but easily done.
Obesity is a method of normalising ATP production. The concept of an adipose tissue "set point" is an artefact of how much adipocyte distension-induced insulin resistance is needed to normalise tissue ATP production at a given level of mitochondrial dysfunction.
Confession time. I never meant anyone to pop a real balloon. You don't have to actually do it. What I really wanted everyone to do was to pin a hypothetical donkey tail to the graph at the top of the post.
You need to guess what the respiratory quotient is for a person who, for the last seven days, has been eating a diet which included less that 20 grams per day of carbohydrate, around 60 grams of protein and as much butter as they like.

All you have to oxidise outside of your brain is fat. Your RQ will plummet to the lowest value possible short of full starvation. FFA delivery to non neural tissue will rocket. Glucose delivery will be irrelevant and the role of insulin in energy production will be sidelined. Cytosolic FFA derivatives will sky rocket too, to keep you alive using physiological insulin resistance, dontcha-no.
Perhaps you will normalise your ATP production?
Might you normalise your appetite too as you normalise your ATP production? It happens for many who try it...
Peter
I think ATP, AMP and AMPK might be an interesting subject to move on to next.