I've been meaning to post on this paper for a long time. It's old but not ancient (2006). The authors are interesting. Collier CA is first author and does not appear to have published anything else, ever. My guess is that it was her PhD which produced the paper and she dropped out of science at this point. Anyone who has tried to get funding for their first post doc will understand. Second author is Bruce CR and he has no other publications on metformin. Smith AC has one other publication on metformin but she wasn't looking at anything interesting from the Protons point of view. Last two authors are group leaders and have virtually zero publications on metformin.
So the lab dabbled in metformin for one PhD and lost either interest or funding. The paper has that feel to it. It looks preliminary, it has a few rough edges, the authors didn't appear to have known what the results were going to be before they started. Back in 2006 no one was thinking about mtG3Pdh or had any real idea of how metformin worked.
They used high doses of metformin and supra maximal doses of insulin on freshly isolated muscle tissue from healthy rats fed standard CIAB. So there is a simple black and white effect, nothing subtle. They looked at glucose oxidation and palmitate oxidation in acutely isolated soleus or epitrochlearis muscle. Soleus is a mixed fuel, oxidative muscle, epitrochlearis is glycolytic. Soleus is the one metformin works on. Here's the effect on palmitate oxidation:
One the left, metformin does nothing to suppress palmitate oxidation. No surprise there. On the right, insulin suppresses fatty acid oxidation.
That was one of the best findings in the paper. Never mind the lipophilic concept of obesity. Even if you keep your fatty acids outside of your adipocytes, insulin will suppress fatty acid oxidation in your soleus type muscles (i.e. an awful lot of them).
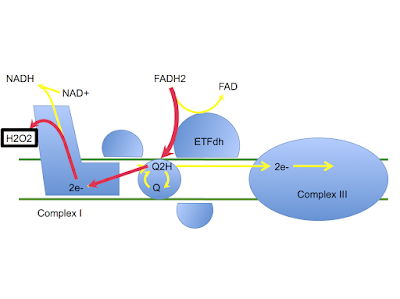
Metformin stops this happening and restores fatty acid oxidation. It does this for all of the reasons in the Protons thread which I won't repeat yet again except to say that, under metformin, insulin signalling can only be facilitated by fatty acid oxidation derived FADH2, not via mtG3Pdh FADH2.
The same happens for glucose oxidation:
Metformin alone does nothing to glucose oxidation in the absence of insulin but it blocks the small increase induced by supramaximal insulin.
If you want to suppress fatty acid oxidation in your muscles, insulin does this very nicely and metformin restores it. This was the most useful finding in the paper.
For whatever reason, they walked away from it.
Peter
Metformin counters the insulin-induced suppression of fatty acid oxidation and stimulation of triacylglycerol storage in rodent skeletal muscle.
Monday, December 28, 2015
Saturday, December 12, 2015
Acetoacetate and arterial oxygen tension
This is very exciting. Remi forwarded it to me. He understands.
Therapeutic ketosis with ketone ester delays central nervous system oxygen toxicity seizures in rats
It’s from D'Agostino’s ketone group. Unless you are in to hyperbaric medicine you can ignore the bulk of the paper. Instead look at Fig. 3:
We're interested in the grey line in graph A with the triangle data points. How does enforced ketosis with an exogenous acetoacetate/betahydroxybutyrate precursor (but not when using a pure beta hydroxybutyrate precursor) raise arterial pO2 from the normal of 100mmHg to the rather spectacular high of 130mmHg?
This is fascinating and of genuine physiological significance. Not the raised arterial pO2 per se, more what it says about AcAc and metabolism. But never the less, how do you get a sustained increase in arterial pO2 by gavaging a with substance which is an AcAc precursor anyway? This is from the discussion:
“An unexpected finding was that BD-AcAc2 [the acetoacetate precursor] caused a significant and sustained increase in blood pO2 levels of ∼30%. It’s conceivable that these changes in PO2 result from BD-AcAc2-induced alterations in the neural control of autonomic regulation, including cardiorespiratory function (38). Further studies are needed to determine the specific contribution of BD-AcAc2 on brain O2 consumption, ventilatory drive, systemic blood pressure, and brain blood flow preceding CNS-OT.”
The finding was unexpected. There is no obvious explanation. It needs further study.
I love this. I’ll put on my anaesthetist’s hat and speculate.
The rats are breathing room air and there is nothing to suggest there has been any change in minute volume of breathing following treatment with the AcAc precursor. I think the effect possibly comes down to a decrease in tissue oxygen consumption under this drug derived ketone.
Aside: pO2 here is the partial pressure of oxygen in the arterial blood. This is only linked to oxygen content via the the oxygen-haemoglobin dissociation curve which is highly non linear. A change in pO2 from 100mmHg to 130mmHg is on the flat section of the curve and adds almost no oxygen carriage/delivery via haemoglobin. But it tells us things. End aside.
If you have a manoeuvre which decreases tissue oxygen consumption but leaves all else unchanged you will raise the partial pressure of oxygen in the alveoli within the lungs closer to the inspired concentration. This is because less is being taken up in to the blood, so more is left in those alveoli. Arterial blood leaving the lungs (in equilibrium with the alveolar pO2) will, therefore, have a higher partial pressure of oxygen too.
Equally, if you have lower oxygen consumption then the partial pressure of oxygen in the venous blood will be raised compared to normal tissue extraction, all other factors being unchanged. Again, it's because less is extracted, more is left. So there will be a higher venous oxygen partial pressure. Now, lungs are not 100% efficient. Some venous blood gets through and lowers the oxygen partial pressure in arterial blood. Higher oxygen partial pressure in venous blood means less effect on arterial blood pO2 through this lung inefficiency.
These are gross simplifications. John Nunn's Applied Respiratory Physiology, chapter 10 p242 onwards, "The oxygen cascade" has a little more detail. OK, a hell of a lot more, caveats included. Especially Fig 10.7.
Is this enough to explain D'Agostino's results? I don’t know. But an idea of whether I am correct would be given by taking a venous blood sample and measuring the venous pO2. The measured effect on arterial pO2 is large so you could possibly see a raised venous pO2 on a simple jugular vein sample without needing to try and get a pulmonary artery sample from a rat. That would give a “back of an envelope” assessment in little more time than it takes time to stick the sample through their blood gas analyser.
Equally, just stick a rat in respiratory chamber, gavage it with the acetoacetate precursor and measure its decrease in O2 uptake.
This finding has huge implications for managing any condition where oxygen delivery is compromised. Not the carotid pO2 of 130mmHg per se, this will have put very little more O2 on to haemoglobin than a pO2 of 100mmHg as stated. It's that decreased need for oxygen by the tissues which it signifies. Acetoacetate appears to allow tissues to function with a significantly reduced need for oxygen; that I find exciting. OK, I'm a bit strange but, well, that's me!
Peter
Summary: People climbing Everest should be in ketosis. With acetoacetate predominating.
Therapeutic ketosis with ketone ester delays central nervous system oxygen toxicity seizures in rats
It’s from D'Agostino’s ketone group. Unless you are in to hyperbaric medicine you can ignore the bulk of the paper. Instead look at Fig. 3:
We're interested in the grey line in graph A with the triangle data points. How does enforced ketosis with an exogenous acetoacetate/betahydroxybutyrate precursor (but not when using a pure beta hydroxybutyrate precursor) raise arterial pO2 from the normal of 100mmHg to the rather spectacular high of 130mmHg?
This is fascinating and of genuine physiological significance. Not the raised arterial pO2 per se, more what it says about AcAc and metabolism. But never the less, how do you get a sustained increase in arterial pO2 by gavaging a with substance which is an AcAc precursor anyway? This is from the discussion:
“An unexpected finding was that BD-AcAc2 [the acetoacetate precursor] caused a significant and sustained increase in blood pO2 levels of ∼30%. It’s conceivable that these changes in PO2 result from BD-AcAc2-induced alterations in the neural control of autonomic regulation, including cardiorespiratory function (38). Further studies are needed to determine the specific contribution of BD-AcAc2 on brain O2 consumption, ventilatory drive, systemic blood pressure, and brain blood flow preceding CNS-OT.”
The finding was unexpected. There is no obvious explanation. It needs further study.
I love this. I’ll put on my anaesthetist’s hat and speculate.
The rats are breathing room air and there is nothing to suggest there has been any change in minute volume of breathing following treatment with the AcAc precursor. I think the effect possibly comes down to a decrease in tissue oxygen consumption under this drug derived ketone.
Aside: pO2 here is the partial pressure of oxygen in the arterial blood. This is only linked to oxygen content via the the oxygen-haemoglobin dissociation curve which is highly non linear. A change in pO2 from 100mmHg to 130mmHg is on the flat section of the curve and adds almost no oxygen carriage/delivery via haemoglobin. But it tells us things. End aside.
If you have a manoeuvre which decreases tissue oxygen consumption but leaves all else unchanged you will raise the partial pressure of oxygen in the alveoli within the lungs closer to the inspired concentration. This is because less is being taken up in to the blood, so more is left in those alveoli. Arterial blood leaving the lungs (in equilibrium with the alveolar pO2) will, therefore, have a higher partial pressure of oxygen too.
Equally, if you have lower oxygen consumption then the partial pressure of oxygen in the venous blood will be raised compared to normal tissue extraction, all other factors being unchanged. Again, it's because less is extracted, more is left. So there will be a higher venous oxygen partial pressure. Now, lungs are not 100% efficient. Some venous blood gets through and lowers the oxygen partial pressure in arterial blood. Higher oxygen partial pressure in venous blood means less effect on arterial blood pO2 through this lung inefficiency.
These are gross simplifications. John Nunn's Applied Respiratory Physiology, chapter 10 p242 onwards, "The oxygen cascade" has a little more detail. OK, a hell of a lot more, caveats included. Especially Fig 10.7.
Is this enough to explain D'Agostino's results? I don’t know. But an idea of whether I am correct would be given by taking a venous blood sample and measuring the venous pO2. The measured effect on arterial pO2 is large so you could possibly see a raised venous pO2 on a simple jugular vein sample without needing to try and get a pulmonary artery sample from a rat. That would give a “back of an envelope” assessment in little more time than it takes time to stick the sample through their blood gas analyser.
Equally, just stick a rat in respiratory chamber, gavage it with the acetoacetate precursor and measure its decrease in O2 uptake.
This finding has huge implications for managing any condition where oxygen delivery is compromised. Not the carotid pO2 of 130mmHg per se, this will have put very little more O2 on to haemoglobin than a pO2 of 100mmHg as stated. It's that decreased need for oxygen by the tissues which it signifies. Acetoacetate appears to allow tissues to function with a significantly reduced need for oxygen; that I find exciting. OK, I'm a bit strange but, well, that's me!
Peter
Summary: People climbing Everest should be in ketosis. With acetoacetate predominating.
Monday, December 07, 2015
Protons (42) Metformin as the next epilepsy drug?
Some things which are written in stone are not quite as they seem. In a chat to karl about metformin/lactate in the brain I started thinking about the control of glucose derived calories being delivered to neurons. There is a general understanding that the brain does not use insulin signalling to control glucose entry to neurons, just as it doesn’t oxidise fatty acids. However we know that astrocytes certainly oxidise fatty acids to ketones and feed those ketones to the neurons, so the old chestnut about the "brain" not oxidising fatty acids is rather limited in its application. Does the same apply to glycolysis and glucose ingress? What about glial cells and insulin signalling?
So I pulled out this paper dated to August this year:
Insulin and IGF1 signalling pathways in human astrocytes in vitro and in vivo; characterisation, subcellular localisation and modulation of the receptors.
It’s a beautiful example of massively clever people who never ask the correct question. I opened the full text and slogged through reams and reams of alphabet soup about insulin signalling in astrocytes. The group are probably planning on maintaining funding by linking modifications of this "alphabet soup" to the development of type 3 diabetes, Alzheimer’s Disease. Great plan.
Of course personally I’m looking for changes in glucose metabolism related to insulin signalling. There is a sh!t load of mtG3Pdh in the mitochondria extracted from homogenised brain tissue and clearly it's doing something there. And that something, as far as I’m concerned, is related to linking glucose ingress to insulin signalling. The initiation and curtailing of insulin signalling in relationship to glucose flux.
After some time spent in the mire of alphabet soup I eventually searched the paper using “glucose” to see if I was missing some deep insight amidst the said alphabet soup.
No. glucose is only mentioned twice. The in-text the mention is irrelevant (talking about hepatic-like cell insulin resistance under fructose). The second mention is in a reference. This is a gem. Back in 1984 we knew this:
Insulin binds to specific receptors and stimulates 2-deoxy-D-glucose uptake in cultured glial cells from rat brain.
I would expect high levels of mtG3Pdh to be associated with very tight regulation of the glucose metabolism mediated through insulin signalling. Not in neurons. Neurons should use lactate. Glycolysis, especially the side-spur to the glycerophosphate shuttle, should be a pathway of last resort for neurons.
Not so in astrocytes. They should really, really tightly control the flux of glucose through themselves as they are the guardians of the neurons. They should meter insulin signalling to control lactate generation for supply to neurons.
Trying to link insulin signalling to Alzheimer’s Disease, without looking at glucose metabolism, leaves you wallowing in an alphabet soup with no way of generating a plan other than to develop some drug or other to block a downstream effect of one of those signalling molecules.
Will modifying the alphabet soup, without providing normoglycaemia, help anything? Well, yes, it will help generate funding.
Prevent AD?
Hahahahahahahaha.
This whole train of thought began with an email from karl linking to this is the editorial:
Fermenting Seizures With Lactate Dehydrogenase
Which discusses a particular paper (no abstract and one author disappeared between NEJM and PubMed, wtf????):
Inhibition of Lactate Dehydrogenase to Treat Epilepsy.
I've not read the text but the editorial is pretty clear about what they did. Does blockade of lactate dehydrogenase reduce seizures? Yes. But my suspicion is only if the astrocytes/glial cells are being driven hard through glycolysis either in tissue culture (at the "normal" high glucose levels used) or in mice fed crapinabag.
Summary: Lactate dehydrogenase feeds lactate from glial cells to neurons. This is Good. Blocking LDH will control seizures if they are being triggered by over supply of hyperglycaemia derived lactate from astrocytes. Metformin might do the same through all of the Protons logical reasons, ie it delays/limits insulin signalling until fatty acid oxidation replaces the glycerophosphate shuttle. By which time there will be increased beta oxidation leading to glial cell ketone generation... So, metformin SHOULD limit seizures if it promotes glial cell beta oxidation to ketones and reduces excess lactate by limiting insulin signalling. That metformin lowers blood glucose would help too.
Well, whoodathunkit?
Peter
Some text-hidden links:
Role of carnitine palmitoyltransferase I in the control of ketogenesis in primary cultures of rat astrocytes.
Roles and regulation of ketogenesis in cultured astroglia and neurons under hypoxia and hypoglycemia.
Metformin protects against seizures, learning and memory impairments and oxidative damage induced by pentylenetetrazole-induced kindling in mice.
So I pulled out this paper dated to August this year:
Insulin and IGF1 signalling pathways in human astrocytes in vitro and in vivo; characterisation, subcellular localisation and modulation of the receptors.
It’s a beautiful example of massively clever people who never ask the correct question. I opened the full text and slogged through reams and reams of alphabet soup about insulin signalling in astrocytes. The group are probably planning on maintaining funding by linking modifications of this "alphabet soup" to the development of type 3 diabetes, Alzheimer’s Disease. Great plan.
Of course personally I’m looking for changes in glucose metabolism related to insulin signalling. There is a sh!t load of mtG3Pdh in the mitochondria extracted from homogenised brain tissue and clearly it's doing something there. And that something, as far as I’m concerned, is related to linking glucose ingress to insulin signalling. The initiation and curtailing of insulin signalling in relationship to glucose flux.
After some time spent in the mire of alphabet soup I eventually searched the paper using “glucose” to see if I was missing some deep insight amidst the said alphabet soup.
No. glucose is only mentioned twice. The in-text the mention is irrelevant (talking about hepatic-like cell insulin resistance under fructose). The second mention is in a reference. This is a gem. Back in 1984 we knew this:
Insulin binds to specific receptors and stimulates 2-deoxy-D-glucose uptake in cultured glial cells from rat brain.
I would expect high levels of mtG3Pdh to be associated with very tight regulation of the glucose metabolism mediated through insulin signalling. Not in neurons. Neurons should use lactate. Glycolysis, especially the side-spur to the glycerophosphate shuttle, should be a pathway of last resort for neurons.
Not so in astrocytes. They should really, really tightly control the flux of glucose through themselves as they are the guardians of the neurons. They should meter insulin signalling to control lactate generation for supply to neurons.
Trying to link insulin signalling to Alzheimer’s Disease, without looking at glucose metabolism, leaves you wallowing in an alphabet soup with no way of generating a plan other than to develop some drug or other to block a downstream effect of one of those signalling molecules.
Will modifying the alphabet soup, without providing normoglycaemia, help anything? Well, yes, it will help generate funding.
Prevent AD?
Hahahahahahahaha.
This whole train of thought began with an email from karl linking to this is the editorial:
Fermenting Seizures With Lactate Dehydrogenase
Which discusses a particular paper (no abstract and one author disappeared between NEJM and PubMed, wtf????):
Inhibition of Lactate Dehydrogenase to Treat Epilepsy.
I've not read the text but the editorial is pretty clear about what they did. Does blockade of lactate dehydrogenase reduce seizures? Yes. But my suspicion is only if the astrocytes/glial cells are being driven hard through glycolysis either in tissue culture (at the "normal" high glucose levels used) or in mice fed crapinabag.
Summary: Lactate dehydrogenase feeds lactate from glial cells to neurons. This is Good. Blocking LDH will control seizures if they are being triggered by over supply of hyperglycaemia derived lactate from astrocytes. Metformin might do the same through all of the Protons logical reasons, ie it delays/limits insulin signalling until fatty acid oxidation replaces the glycerophosphate shuttle. By which time there will be increased beta oxidation leading to glial cell ketone generation... So, metformin SHOULD limit seizures if it promotes glial cell beta oxidation to ketones and reduces excess lactate by limiting insulin signalling. That metformin lowers blood glucose would help too.
Well, whoodathunkit?
Peter
Some text-hidden links:
Role of carnitine palmitoyltransferase I in the control of ketogenesis in primary cultures of rat astrocytes.
Roles and regulation of ketogenesis in cultured astroglia and neurons under hypoxia and hypoglycemia.
Metformin protects against seizures, learning and memory impairments and oxidative damage induced by pentylenetetrazole-induced kindling in mice.
Friday, November 27, 2015
Protons (41) Metformin in the liver
Just a brief note on metformin. No need for detailed analysis as there's not much to argue with. I think they are correct, even if we have differing views of the function of the glycerophosphate shuttle.
Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase
The paper makes a pretty good case for the action of metformin, at pharmacologically appropriate concentrations, as being to inhibit mtG3Pdh. At higher concentrations it undoubtedly inhibits complex I but its action at the glycerophosphate shuttle makes a great deal more sense. In the last post I looked at the inhibition of this shuttle as an inhibitor of glucose signalling which could be rescued by adequate fatty acid oxidation in the peripheral tissues. This too would undoubtedly be a critical action and I'll come back to it later.
I'd just like to emphasise first that the suppression of hepatic glucose output is also controlled by the redox state of the cytoplasm. In a normal liver cell a side spur of glycolysis drives enough electrons in to the ETC at mtG3Pdh to activate insulin signalling and concurrently reduces NADH while increasing NAD+. The rising level of NADH under metformin (due to blocking this oxidation of NADH) makes the conversion of lactate to pyruvate energetically impossible and so lactate derived gluconeogenesis stops on a redox basis. The conversion of glycerol to glucose via glycerol-3-phosphate is impossible using mtG3Pdh because metformin specifically blocks this enzyme. Some gluconeogenesis is quite possible via pyruvate, via alanine and other amino acids and, if you supply it, via dihydroxyacetone. But the paper suggests that redox change and enzyme inhibition underly the drop in hepatic glucose output seen with metformin. Fresh liver cells with or without metformin trying to generate glucose from various substrates gives us this picture:
Other parts of the paper were good too and I particularly enjoyed the forced change in lactate:pyruvate ratio in the culture medium section which mimicked metformin's action, but I think that's enough on modern views of metformin acting on the liver. I accept it works through inhibiting mtG3Pdh and subsequent change in redox status. Next proper post will be some ancient history from 9 years ago looking at muscles and metformin, where the Protons ideas from the last post get some support.
Peter
Summary: Metformin suppresses hepatic glucose output through decreased gluconeogenesis by inhibiting mtG3Pdh. Lots of evidence.
Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase
The paper makes a pretty good case for the action of metformin, at pharmacologically appropriate concentrations, as being to inhibit mtG3Pdh. At higher concentrations it undoubtedly inhibits complex I but its action at the glycerophosphate shuttle makes a great deal more sense. In the last post I looked at the inhibition of this shuttle as an inhibitor of glucose signalling which could be rescued by adequate fatty acid oxidation in the peripheral tissues. This too would undoubtedly be a critical action and I'll come back to it later.
I'd just like to emphasise first that the suppression of hepatic glucose output is also controlled by the redox state of the cytoplasm. In a normal liver cell a side spur of glycolysis drives enough electrons in to the ETC at mtG3Pdh to activate insulin signalling and concurrently reduces NADH while increasing NAD+. The rising level of NADH under metformin (due to blocking this oxidation of NADH) makes the conversion of lactate to pyruvate energetically impossible and so lactate derived gluconeogenesis stops on a redox basis. The conversion of glycerol to glucose via glycerol-3-phosphate is impossible using mtG3Pdh because metformin specifically blocks this enzyme. Some gluconeogenesis is quite possible via pyruvate, via alanine and other amino acids and, if you supply it, via dihydroxyacetone. But the paper suggests that redox change and enzyme inhibition underly the drop in hepatic glucose output seen with metformin. Fresh liver cells with or without metformin trying to generate glucose from various substrates gives us this picture:
Other parts of the paper were good too and I particularly enjoyed the forced change in lactate:pyruvate ratio in the culture medium section which mimicked metformin's action, but I think that's enough on modern views of metformin acting on the liver. I accept it works through inhibiting mtG3Pdh and subsequent change in redox status. Next proper post will be some ancient history from 9 years ago looking at muscles and metformin, where the Protons ideas from the last post get some support.
Peter
Summary: Metformin suppresses hepatic glucose output through decreased gluconeogenesis by inhibiting mtG3Pdh. Lots of evidence.
Friday, November 20, 2015
Protons (40) Living without the glycerophosphate shuttle
If we look at a mouse with a deletion of the gene for cytoplasmicG3Pdh we have a reasonable model for elimination of the glycerophosphate shuttle at the level were glycolysis would normally be used to drive reverse electron flow through complex I, to facilitate insulin signalling. These mice are remarkably normal and can swim in deep water, possibly not too happily, for at least 20 minutes with weights on their tails, i.e. they can exercise, at least if necessary to save their lives. They have markedly reduced levels of pyruvate and mildly elevated levels of lactate in muscle tissue compared to control mice.
It's the bottom two lines which I looked at. The lactate to pyruvate ratio reflects the NADH to NAD+ ratio within the cytoplasm, as Krebs puts it:
In a cell [H+] is a constant and K is also a constant (by definition).
So clearly we have a lot more NADH available in the knockout mouse, so more lactate gets formed from pyruvate, which becomes a minor player in the cascade of glycolysis to oxidative phosphorylation allowing lactate to take over. The authors of the mouse paper suggest that the lactate is expelled from the cells and that the Cori cycle, in the liver, is active to deal with the it. I’d prefer to think of lactate as being shunted directly to the mitochondria for use in the TCA.
If you subscribe to the view that the glycerophosphate shuttle is needed to provide NAD+ for glycolysis to proceed you might expect a few problems with glucose processing. There is undoubtedly an accumulation of metabolites upstream of the glycerophosphate shuttle and a depletion of those downstream but glycolysis does proceed. But from my point of view, with no glycerophosphate shuttle, there is nothing to allow the body to facilitate insulin’s drive to self activate using glucose. How do these mice cope?
They cope very well.
If you feel that tying a weight to the tail of a mouse and dropping it a beaker of water is a bit too crude, there are more sophisticated methods of inducing exercise. Worse than making obese people do cardio at any gym where fat shaming rules. It's possible to run a mouse to utter exhaustion and monitor its respiratory quotient while it runs. So you can see whether it burns predominantly glucose or fat and in what balance. You can also measure exactly how long it can run for, before it collapses at the level of exhaustion where it can no longer avoid an electroshock or two or three. Here are the core findings from sending mice to an electro-gym (the Thumb Tack Hypothesis taken to serious levels):
HeA are the knockout mice, By are the control mice. Knockout mice run harder and for longer than control mice. The rest of the graphs use the same coding, solid line is the control mice, dotted line the knockouts.
Taken from the RQ we can ask whether the knockout mice can oxidise glucose. Yes:
Pretty much as well as the control mice.
Can they oxidise lipid? Yes, somewhat better than can the control mice:
I think it is also worth noting that under marked but non-exhausting exercise that glycogen in the muscle of knockout mice does not fall, it does so in control mice:
These modified mice, which cannot use glycolysis to trigger insulin signalling, have a tendency to have MORE glycogen in their muscles (although p is greater than 0.05) at rest and they deplete it less under sustained near-maximal exercise. I'd guess insulin does signal.
It's also worth noting that blood lactate under the same conditions does not rise in the knockout mice whereas it does in control mice (p less than 0.05, yay!). My assumption is that lactate is being metabolised in the muscles of knockout mice and shunted to the liver for the Cori Cycle in control mice:
So what might be going on in these knockout mice? The requirement for insulin signalling is a modest amount of reverse flow of electrons through complex I, ie the CoQ couple must be reduced. The usual, here absent, technique is the glycerophosphate shuttle. But we can reduce the CoQ couple in other ways. My favourite way is via the oxidation of the FADH2 generated by metabolism of saturated fatty acids. How much FADH2 is needed to replace the glycerophosphate shuttle?
From the graph of lipid oxidation above we can see that knockout mice under exercise are oxidising somewhere around 45mg/kg/min of fat. The control mice are oxidising just over 30mg/kg/min. From the Protons perspective the increased fat oxidation is a requirement for normal insulin signalling and this insulin signal cannot limit fatty acid oxidation until the rate is almost 50% higher in the knockout mice than in those where the glycerophosphate shuttle works. These mice oxidise fat because insulin signalling is not being triggered by glycolysis. It also means that lipid oxidation has to be higher before it can trigger insulin resistance and cellular energy influx limitation.
We don't (as far as I know) have a drug to inhibit cytG3Pdh.
We do have one to inhibit mtG3Pdh, the other half of the glycerophosphate shuttle.
It's called metformin. Does metformin do the same thing as having a cytG3Pdh knockout does? Under exercise? In terms of getting the King Of the Mountains jersey in the Tour de France perhaps?
Possibly so.
Peter
Summary: Metformin blocks glycolysis triggered insulin signalling and cells replace this with FADH2 triggered insulin signalling from fatty acid oxidation (at ETFdh). This results increased fatty acid oxidation and in improved high intensity exercise ability. Oh, and I guess weight loss etc...
Aside. I think I might start sticking the refs from a post in at the end. There are times I can't remember in which post a paper was used, searching my own blog/hard drive might be easier if the author or a keyword are actually present rather than there just being a highlighted text field!!! The blog is getting a bit unwieldy.
Glycerol 3-phosphate dehydrogenase 1 deficiency enhances exercise capacity due to increased lipid oxidation during strenuous exercise
Mouse lacking NAD+-linked glycerol phosphate dehydrogenase has normal pancreatic beta cell function but abnormal metabolite pattern in skeletal muscle
The Redox State of Free Nicotinamide-Adenine Dinucleotide in the Cytoplasm and Mitochondria of Rat Liver
Metformin improves performance in high-intensity exercise, but not anaerobic capacity in healthy male subjects.
It's the bottom two lines which I looked at. The lactate to pyruvate ratio reflects the NADH to NAD+ ratio within the cytoplasm, as Krebs puts it:
In a cell [H+] is a constant and K is also a constant (by definition).
So clearly we have a lot more NADH available in the knockout mouse, so more lactate gets formed from pyruvate, which becomes a minor player in the cascade of glycolysis to oxidative phosphorylation allowing lactate to take over. The authors of the mouse paper suggest that the lactate is expelled from the cells and that the Cori cycle, in the liver, is active to deal with the it. I’d prefer to think of lactate as being shunted directly to the mitochondria for use in the TCA.
If you subscribe to the view that the glycerophosphate shuttle is needed to provide NAD+ for glycolysis to proceed you might expect a few problems with glucose processing. There is undoubtedly an accumulation of metabolites upstream of the glycerophosphate shuttle and a depletion of those downstream but glycolysis does proceed. But from my point of view, with no glycerophosphate shuttle, there is nothing to allow the body to facilitate insulin’s drive to self activate using glucose. How do these mice cope?
They cope very well.
If you feel that tying a weight to the tail of a mouse and dropping it a beaker of water is a bit too crude, there are more sophisticated methods of inducing exercise. Worse than making obese people do cardio at any gym where fat shaming rules. It's possible to run a mouse to utter exhaustion and monitor its respiratory quotient while it runs. So you can see whether it burns predominantly glucose or fat and in what balance. You can also measure exactly how long it can run for, before it collapses at the level of exhaustion where it can no longer avoid an electroshock or two or three. Here are the core findings from sending mice to an electro-gym (the Thumb Tack Hypothesis taken to serious levels):
HeA are the knockout mice, By are the control mice. Knockout mice run harder and for longer than control mice. The rest of the graphs use the same coding, solid line is the control mice, dotted line the knockouts.
Taken from the RQ we can ask whether the knockout mice can oxidise glucose. Yes:
Pretty much as well as the control mice.
Can they oxidise lipid? Yes, somewhat better than can the control mice:
I think it is also worth noting that under marked but non-exhausting exercise that glycogen in the muscle of knockout mice does not fall, it does so in control mice:
These modified mice, which cannot use glycolysis to trigger insulin signalling, have a tendency to have MORE glycogen in their muscles (although p is greater than 0.05) at rest and they deplete it less under sustained near-maximal exercise. I'd guess insulin does signal.
It's also worth noting that blood lactate under the same conditions does not rise in the knockout mice whereas it does in control mice (p less than 0.05, yay!). My assumption is that lactate is being metabolised in the muscles of knockout mice and shunted to the liver for the Cori Cycle in control mice:
So what might be going on in these knockout mice? The requirement for insulin signalling is a modest amount of reverse flow of electrons through complex I, ie the CoQ couple must be reduced. The usual, here absent, technique is the glycerophosphate shuttle. But we can reduce the CoQ couple in other ways. My favourite way is via the oxidation of the FADH2 generated by metabolism of saturated fatty acids. How much FADH2 is needed to replace the glycerophosphate shuttle?
From the graph of lipid oxidation above we can see that knockout mice under exercise are oxidising somewhere around 45mg/kg/min of fat. The control mice are oxidising just over 30mg/kg/min. From the Protons perspective the increased fat oxidation is a requirement for normal insulin signalling and this insulin signal cannot limit fatty acid oxidation until the rate is almost 50% higher in the knockout mice than in those where the glycerophosphate shuttle works. These mice oxidise fat because insulin signalling is not being triggered by glycolysis. It also means that lipid oxidation has to be higher before it can trigger insulin resistance and cellular energy influx limitation.
We don't (as far as I know) have a drug to inhibit cytG3Pdh.
We do have one to inhibit mtG3Pdh, the other half of the glycerophosphate shuttle.
It's called metformin. Does metformin do the same thing as having a cytG3Pdh knockout does? Under exercise? In terms of getting the King Of the Mountains jersey in the Tour de France perhaps?
Possibly so.
Peter
Summary: Metformin blocks glycolysis triggered insulin signalling and cells replace this with FADH2 triggered insulin signalling from fatty acid oxidation (at ETFdh). This results increased fatty acid oxidation and in improved high intensity exercise ability. Oh, and I guess weight loss etc...
Aside. I think I might start sticking the refs from a post in at the end. There are times I can't remember in which post a paper was used, searching my own blog/hard drive might be easier if the author or a keyword are actually present rather than there just being a highlighted text field!!! The blog is getting a bit unwieldy.
Glycerol 3-phosphate dehydrogenase 1 deficiency enhances exercise capacity due to increased lipid oxidation during strenuous exercise
Mouse lacking NAD+-linked glycerol phosphate dehydrogenase has normal pancreatic beta cell function but abnormal metabolite pattern in skeletal muscle
The Redox State of Free Nicotinamide-Adenine Dinucleotide in the Cytoplasm and Mitochondria of Rat Liver
Metformin improves performance in high-intensity exercise, but not anaerobic capacity in healthy male subjects.
Wednesday, October 28, 2015
Protons (39) mtG3Pdh and lactate vs pyruvate
Here is a schematic illustration of the generation of lactate from glucose as suggested by Schurr, ready for doodling on:
In more artistic style, from Figure 1 in Schurr's paper, it looks like this:
If we look at the more traditional view of glycolysis to pyruvate with a deficit of NAD+ which must be made up by the mtG3Pdh enzyme we have something which looks quite like this:
The concept here is that mtG3Pdh is being used to regenerate the NAD+ which is essential for glycolysis to proceed to pyruvate. Of course, this concept becomes obsolete as soon as we adopt the lactate hypothesis. I tend to view reality as a combination of two pathways like this:
Normal function is via lactate with NAD+ and NADH in perfect balance. The generation of NAD+ from NADH by mtG3Pdh reduces the redox potential of the cytoplasm so the drive to generate lactate, while NADH is in short supply, becomes unhelpful or frankly impossible. For each NADH utilised by mtG3Pdh it is necessary to abort glycolysis at pyruvate, saving the one equivalent NADH by terminating it here rather than at lactate.
It's not that mtG3Pdh replenishes essential NAD+, it's that its consumption of NADH obliges termination of glycolysis at pyruvate. So is mtG3Pdh doing, if the traditional view is a load of bollocks?
Insulin signalling:
Under conditions of high glucose throughput, with insulin signalling, glycolysis will terminate at pyruvate in proportion to the activation of the glycerophosphate shuttle. Notice the two blue arrows signifying two actions of insulin. If we go back to Veech once more, with his isolated heart preparations, we have these two very specific actions of insulin:
One is an increase in glycogen synthesis. Flooding cardiac myocytes with insulin puts every GLUT4 possible on to the cell surface and intracellular glucose approaches that of the perfusing buffer, in this case 10mmol/l. The cells have absolutely no use for this much suddenly available glucose and the simple solution is to divert it to glycogen. The use of intensive insulin therapy in humans with T2D always improves non-oxidative glucose disposal. It goes to glycogen. They get fat too of course. I guess we could quote Veech's abstract:
"The administration of saturating doses of insulin to the glucose perfused, working rat heart acutely increased activity of the glucose transporter 4, GLUT 4, in the plasma membrane (equilibrating extracellular glucose and intracellular [glucose]), activated glycogen synthase (stimulating the rate of glycogen synthesis), and increased mitochondrial acetyl CoA production by the pyruvate
dehydrogenase multienzyme complex. Unexpectedly, insulin increased cardiac hydraulic work but decreased net glycolytic flux and O2 consumption, improving net cardiac efficiency by 28%".
The second arrow points to the mitochondria. Insulin acts to produce a covalent change in the ETC proteins which improves ATP generation per unit oxygen consumed.
In Veech's isolated rat heart preparation insulin REDUCES glycolysis, increases glycogen synthesis and increases mitochondrial ETC efficiency. It's all in the paper on the link above and in assorted related papers, many of which are free full texts and cover the basics. And not so basics.
Veech was looking at combinations of glucose, insulin and ketone bodies. Unlike myself, he is no lover of fatty acids. Ah well. So the buffer used had no fatty acids at all. Now, what do we think insulin will do to fatty acids? It has already maximised the efficiency of the ETC and shunted excess glucose to (harmless) glycogen.
Does insulin facilitate or inhibit the oxidation of fatty acids? The process is just like the diversion of glucose to glycogen:
Once upon a time, before insulin kicked in, CPT1 was used to supply fatty acids to the mitochondria for beta oxidation. Given the increased efficiency of ox phos under insulin, the fate of a significant proportion of fatty acids presenting for beta oxidation is to meet a blockade at CPT1 and to be diverted towards re esterification to triglycerides in the cytoplasm.
I wouldn't suggest that intramuscular triglycerides cause insulin resistance per se. But derivatives there-of do appear to do so and there is certainly an association between intramyocyte triglyceride accumulation and insulin resistance, particularly in non athletes.
This all well and good. Things become more interesting when we take a mtG3Pdh knockout mouse, which cannot signal through mtG3Pdh, and make it run. And run. And run. Until exhaustion, whenever that might be. Of course we also have a rather popular drug to inhibit mtG3Pdh which might mimic the knockout situation. Perhaps for the next post.
Peter
In more artistic style, from Figure 1 in Schurr's paper, it looks like this:
If we look at the more traditional view of glycolysis to pyruvate with a deficit of NAD+ which must be made up by the mtG3Pdh enzyme we have something which looks quite like this:
The concept here is that mtG3Pdh is being used to regenerate the NAD+ which is essential for glycolysis to proceed to pyruvate. Of course, this concept becomes obsolete as soon as we adopt the lactate hypothesis. I tend to view reality as a combination of two pathways like this:
Normal function is via lactate with NAD+ and NADH in perfect balance. The generation of NAD+ from NADH by mtG3Pdh reduces the redox potential of the cytoplasm so the drive to generate lactate, while NADH is in short supply, becomes unhelpful or frankly impossible. For each NADH utilised by mtG3Pdh it is necessary to abort glycolysis at pyruvate, saving the one equivalent NADH by terminating it here rather than at lactate.
It's not that mtG3Pdh replenishes essential NAD+, it's that its consumption of NADH obliges termination of glycolysis at pyruvate. So is mtG3Pdh doing, if the traditional view is a load of bollocks?
Insulin signalling:
Under conditions of high glucose throughput, with insulin signalling, glycolysis will terminate at pyruvate in proportion to the activation of the glycerophosphate shuttle. Notice the two blue arrows signifying two actions of insulin. If we go back to Veech once more, with his isolated heart preparations, we have these two very specific actions of insulin:
One is an increase in glycogen synthesis. Flooding cardiac myocytes with insulin puts every GLUT4 possible on to the cell surface and intracellular glucose approaches that of the perfusing buffer, in this case 10mmol/l. The cells have absolutely no use for this much suddenly available glucose and the simple solution is to divert it to glycogen. The use of intensive insulin therapy in humans with T2D always improves non-oxidative glucose disposal. It goes to glycogen. They get fat too of course. I guess we could quote Veech's abstract:
"The administration of saturating doses of insulin to the glucose perfused, working rat heart acutely increased activity of the glucose transporter 4, GLUT 4, in the plasma membrane (equilibrating extracellular glucose and intracellular [glucose]), activated glycogen synthase (stimulating the rate of glycogen synthesis), and increased mitochondrial acetyl CoA production by the pyruvate
dehydrogenase multienzyme complex. Unexpectedly, insulin increased cardiac hydraulic work but decreased net glycolytic flux and O2 consumption, improving net cardiac efficiency by 28%".
The second arrow points to the mitochondria. Insulin acts to produce a covalent change in the ETC proteins which improves ATP generation per unit oxygen consumed.
In Veech's isolated rat heart preparation insulin REDUCES glycolysis, increases glycogen synthesis and increases mitochondrial ETC efficiency. It's all in the paper on the link above and in assorted related papers, many of which are free full texts and cover the basics. And not so basics.
Veech was looking at combinations of glucose, insulin and ketone bodies. Unlike myself, he is no lover of fatty acids. Ah well. So the buffer used had no fatty acids at all. Now, what do we think insulin will do to fatty acids? It has already maximised the efficiency of the ETC and shunted excess glucose to (harmless) glycogen.
Does insulin facilitate or inhibit the oxidation of fatty acids? The process is just like the diversion of glucose to glycogen:
Once upon a time, before insulin kicked in, CPT1 was used to supply fatty acids to the mitochondria for beta oxidation. Given the increased efficiency of ox phos under insulin, the fate of a significant proportion of fatty acids presenting for beta oxidation is to meet a blockade at CPT1 and to be diverted towards re esterification to triglycerides in the cytoplasm.
I wouldn't suggest that intramuscular triglycerides cause insulin resistance per se. But derivatives there-of do appear to do so and there is certainly an association between intramyocyte triglyceride accumulation and insulin resistance, particularly in non athletes.
This all well and good. Things become more interesting when we take a mtG3Pdh knockout mouse, which cannot signal through mtG3Pdh, and make it run. And run. And run. Until exhaustion, whenever that might be. Of course we also have a rather popular drug to inhibit mtG3Pdh which might mimic the knockout situation. Perhaps for the next post.
Peter
Wednesday, October 14, 2015
Protons (37) full glycerophosphate shuttle knockout mice
Just a short post on this paper:
Lethal Hypoglycemic Ketosis and Glyceroluria in Mice Lacking Both the Mitochondrial and the Cytosolic Glycerol Phosphate Dehydrogenases
The glycerol-3-phosphate shuttle is composed of a cytosolic G3Pdh which actually hydrogenates dihydroxy acetone phosphate to glycerol-3-phosphate, using NADH, and a second, mitochondrial version, which does the actual dehydrogenating reconversion back to dihydroxy acetone phosphate. Assuming things are going in the most usual direction.
Lab models of mice with knockout of either part of the glycerol-3-phosphate shuttle are very interesting and are long term survivors, to be discussed another day. Today I’d just like to think about those mice with a complete knockout, deleting both components. They die at a few days of age with an array of problems, lethal hypoglycaemia being the end crisis.
At this stage of life they are being fed a very high fat, low carbohydrate diet (mouse milk, it's mostly palmitic acid. That should tell you something!) and they are very heavily reliant on gluconeogensis to maintain adequate glucose levels using glycerol from the milk's triglycerides as the necessary glucose precursor. As the paper says:
“Glyceride-glycerol is an especially important gluconeogenic precursor in the neonatal mouse, because 80% of calories from mouse milk are derived from fat, 16–17% from protein, and only 2–5% from lactose (20, 22–24). Thus total calories available from dietary glycerol ( 4%) equal calories from lactose.”
Now, if you are a lab mouse drinking a low carbohydrate diet, should you be insulin sensitive or insulin resistant? If you are insulin sensitive, how much glucose would you like to waste in your muscles, when you only have a limited supply of the stuff in the first place? I would like to suggest that, even in mice, burning glucose for fuel when there is a very limited supply, might not be a survival trait. So insulin resistance, physiological, might be essential for survival. If physiological resistance is essential this is why they have evolved to produce palmitic acid as the main fat in the maternal milk supply. What is needed is a decent input at ETFdh plus and some input at mtG3Pdh to drive enough electrons backwards through complex I to achieve full physiological insulin resistance.
These mice have zero input at mtG3Pdh so are reliant on ETFdh working under palmitic acid to try and achieve this. This clearly doesn't hack it.
The electron transport chain has an ad libitum supply of palmitic acid. The question is:
Without the glycerophosphate shuttle, can the ETC generate reverse electron flow using ETFdh alone to trigger enough superoxide to adequately resist insulin's wasteful usage of precious glucose?
Obviously not. So the second question has to be:
Can pamitic acid at levels in excess of 900micromol/l generate just enough superoxide to allow insulin signalling to commence, without assistance from mtG3Pdh?
I suspect the answer is yes. This generates just enough superoxide (hence H2O2) to allow insulin signalling to commence. Active but inappropriate insulin signalling then triggers a fatal fall in blood glucose as GLUT4s translocate to cell surfaces and glucose drops through them to be squandered irreplaceably. Glucose crashes, the mice die.
It's an extreme model but it makes us think about what might be happening in addition the malonyl-CoA and CPT1 level of signalling and the limited gluconeogenesis discussed so very nicely in the paper.
Peter
Lethal Hypoglycemic Ketosis and Glyceroluria in Mice Lacking Both the Mitochondrial and the Cytosolic Glycerol Phosphate Dehydrogenases
The glycerol-3-phosphate shuttle is composed of a cytosolic G3Pdh which actually hydrogenates dihydroxy acetone phosphate to glycerol-3-phosphate, using NADH, and a second, mitochondrial version, which does the actual dehydrogenating reconversion back to dihydroxy acetone phosphate. Assuming things are going in the most usual direction.
Lab models of mice with knockout of either part of the glycerol-3-phosphate shuttle are very interesting and are long term survivors, to be discussed another day. Today I’d just like to think about those mice with a complete knockout, deleting both components. They die at a few days of age with an array of problems, lethal hypoglycaemia being the end crisis.
At this stage of life they are being fed a very high fat, low carbohydrate diet (mouse milk, it's mostly palmitic acid. That should tell you something!) and they are very heavily reliant on gluconeogensis to maintain adequate glucose levels using glycerol from the milk's triglycerides as the necessary glucose precursor. As the paper says:
“Glyceride-glycerol is an especially important gluconeogenic precursor in the neonatal mouse, because 80% of calories from mouse milk are derived from fat, 16–17% from protein, and only 2–5% from lactose (20, 22–24). Thus total calories available from dietary glycerol ( 4%) equal calories from lactose.”
Now, if you are a lab mouse drinking a low carbohydrate diet, should you be insulin sensitive or insulin resistant? If you are insulin sensitive, how much glucose would you like to waste in your muscles, when you only have a limited supply of the stuff in the first place? I would like to suggest that, even in mice, burning glucose for fuel when there is a very limited supply, might not be a survival trait. So insulin resistance, physiological, might be essential for survival. If physiological resistance is essential this is why they have evolved to produce palmitic acid as the main fat in the maternal milk supply. What is needed is a decent input at ETFdh plus and some input at mtG3Pdh to drive enough electrons backwards through complex I to achieve full physiological insulin resistance.
These mice have zero input at mtG3Pdh so are reliant on ETFdh working under palmitic acid to try and achieve this. This clearly doesn't hack it.
The electron transport chain has an ad libitum supply of palmitic acid. The question is:
Without the glycerophosphate shuttle, can the ETC generate reverse electron flow using ETFdh alone to trigger enough superoxide to adequately resist insulin's wasteful usage of precious glucose?
Obviously not. So the second question has to be:
Can pamitic acid at levels in excess of 900micromol/l generate just enough superoxide to allow insulin signalling to commence, without assistance from mtG3Pdh?
I suspect the answer is yes. This generates just enough superoxide (hence H2O2) to allow insulin signalling to commence. Active but inappropriate insulin signalling then triggers a fatal fall in blood glucose as GLUT4s translocate to cell surfaces and glucose drops through them to be squandered irreplaceably. Glucose crashes, the mice die.
It's an extreme model but it makes us think about what might be happening in addition the malonyl-CoA and CPT1 level of signalling and the limited gluconeogenesis discussed so very nicely in the paper.
Peter
Saturday, October 10, 2015
Protons (38) and ultra low fat once more
OMG, here we go with more doodles. Ah well...
This post is a summary of the ideas which came out of the Protons thread. I’ve been meaning to write it for some time but the trigger was really Denise Minger’s idea of “carbosis”. This has made me revisit ideas I kicked around at the time of the Potato Diet about the systemic level of insulin and revisited within the Protons concept. I guess the idea is to try and work out whether there is any physiologically plausible explanation for the changes seen under ultra low fat eating, under carbosis.
This is my opinion, most of the references are buried in the Protons thread and some ideas I have interpolated from hard facts because they make sense to me. But be aware you are reading an opinion piece.
Cellular insulin response is controlled by superoxide produced at complex I, which exits the mitochondria as H2O2. Small pulses of H2O2 limit the activity of PTP 1B (protein tyrosine phosphatase 1B). Disabling PTP 1B takes the brakes off of the insulin receptor and allows it to autophosphorylate whenever insulin binds and so allows subsequent insulin signalling to take place.
Large amounts of H2O2 inhibit the autophosphorylation of the insulin receptor directly, at several sites, and so cause insulin resistance per se.
So it's pretty obvious that mitochondrial superoxide/H2O2 controls insulin function and subsequent blood glucose levels, and obesity levels if you are a True Believer, which I am. In this post I'd just like to summarise my own personal thoughts on how the electron transport chain, from where much of the the superoxide is produced, behaves under a variety of conditions.
It is quite easy to set up a mitochondrial preparation which can be driven almost completely through complex I. You can feed it on pyruvate/malate. Under these conditions there is essentially zero H2O2 generation, so there is obviously very limited superoxide generation. Think of it like this:
Electrons from NADH simply drop through complex I, fall easily down hill on to the CoQ couple and are handed on to complex III and the rest of the chain. Similarly we can run tissues on pure glucose at modest levels, even if that's not quite how we do it in real life. Many of Veech's papers on ketones used isolated heart preparations which work quite well for quite some time on oxygenated buffer with glucose alone as the sole metabolic substrate, without insulin. So mitochondria can work on pyruvate and isolated hearts can work on pure glucose.
The next piece of input we need to consider is succinate dehydrogenase (SDH), also known as complex II but I'll use SDH as the term in this post. As the TCA turns using one molecule of acetyl-CoA it generates 3 molecules of NADH and one of FADH2, the later being embedded deep within SDH. The FADH2 of succinate dehydrogenase feeds directly to the CoQ couple and reduces it independently of electrons coming from complex I. We have a situation like this:
The TCA is turning and the ETC is accepting input at two points. This is normal physiology and generates very little superoxide, especially while rest of the ETC is well oxidised and so very willing to accept electrons.
With a mitochondrial preparation it is very easy to supply an input of exogenous succinate to SDH without the rest of the TCA cycling in synchrony. This is an experimental situation, only seen in in-tact animals if they are dosed orally with succinc acid esters. This is what happens:
The diagram doesn't make it terribly clear so lets clarify the flow of electrons from SDH, given a sudden massive rise in isolated succinate. Reverse electron flow to superoxide is picked out in red:
Feeding high levels of succinate to a mitochondrial preparation produces massive levels of superoxide. This is not physiology but it can be viewed as a pharmacological demonstration of physiology pushed beyond its normal limits. It's an illustration.
Aside: mitochondria normally oscillate in their function. The TCA drives complex I via NADH (mostly from the early part of the TCA) to the CoQ couple. SDH reduces the CoQ couple independently so opposes this process. Oxaloacetate at the end of the TCA inhibits SDH, facilitating input at complex I, and the whole system goes back and forth as a normal oscillatory process. That's how it is. I’ve no idea why it’s organised this way, but it clearly works rather well! End aside.
But we can say that some degree of reverse electron flow from SDH through complex I will allow small amounts of superoxide generation which will generate modest pulses of H2O2 as far as PTP 1B. This is essential for insulin signalling.
I feel the next step is to look at the situation where glucose is in oversupply, classically after a pure starch meal. Here we need a brake to be applied to the influx of glucose to the cell. In the aftermath of a glucose based meal we would expect insulin to be high, GLUT4s to be active and ox phos to be based on pyruvate (or lactate if you prefer). What is needed is to reduce insulin signalling, limit GLUT4 translocation and so limit glucose ingress to that which is needed by the cell. This is achieved through a side branch of the glycolytic pathway which generates glycerol-3-phosphate. Among the many, many functions of G-3-P, one is to input electrons from NADH to the electron transport chain from the cytoplasmic side of the inner mitochondrial membrane which will reduce the CoQ couple. How much it does this probably depends on the level of metabolites running down through glycolysis. Let's think about a high glycolytic flux, marked reduction of the CoQ couple and see what happens:
The things to note are a large input of cytoplasmic NADH generating marked reverse electron flow through complex I to generate enough superoxide to send H2O2 to inhibit the action of the insulin/receptor complex. It's a simple negative feedback situation and probably produces quite precise control of access of glucose tailored to the needs of the individual cell. There is no pathology here, it's how glucose based metabolism should be controlled.
The next scenario to consider is something like a large ingress of uncontrollable carbohydrate. A find of honey or table sugar. Let's think about it in the complete absence of any fatty acid metabolism. If we have a sudden avalanche of fructose which pours down through glycolysis, what happens? This unstoppable cascade will activate mtG3Pdh much as the excess glucose we have just considered. This should produce a large amount of H2O2 and disable activity of the insulin receptor and produce enough limitation of GLUT4 translocation to exactly limit glucose access by the correct amount to offset the fructose flood. There are other issues from fructose but these are asides. If metabolism is based on pure glycolysis to supply ox phos substrate then fructose can be accommodated by reducing glucose ingress. From the cellular point of view it all balances out and the degree of insulin resistance is at appropriate physiological levels and only occurs while fructose is high, i.e. not for very long. I'll leave uric acid and metabolic syndrome out from the current discussion, needless to say there are issues, for and against.
So I view mtG3Pdh as a balancing act controlling access of carbohydrate to ox phos by controlling insulin signalling through reverse electron transport through complex I. If these are the only components supplying the ETC it seems to be a pretty simple balancing act which might work rather well. On a pure glucose diet some fructose, even quite a lot, is no problem.
Now we have to add in free fatty acids. While beta oxidation generates acetyl CoA and NADH, one molecule of each for each pair of carbon atoms in the chain, they also generate a molecule of FADH2 at the same time. FADH2 is never used as an unbound molecule, here it is stored within electron transporting flavoprotein which delivers FADH2's electrons to the ETC at electron transporting flavoprotein dehydrogenase (ETFdh in the diagram). Much the same as glycerol-3-phosphate at mtG3Pdh, ETFdh reduces the CoQ couple and is adept at driving reverse electron flow through complex I. Low inputs will do nothing or merely generate small pulses of H2O2 at activating levels, high inputs will generate high levels of H2O2 to shut down insulin signalling on the basis that there is plenty of metabolic substrate from fats, minimal glucose is needed, thank you very much. Again, this is pure physiology, I see no pathology in it.
It looks like this:
The step in beta oxidation which produces the FADH2 to drive ETFdh does not occur when the fatty acid being processed presents a double bond at this step. So fully saturated fatty acids generate the maximum amount of FADH2, monounsaturated fats somewhat less and PUFA least of all. The exception is any fatty acids longer than about 18 carbon atoms, these go to peroxisomes rather than mitochondria. So if we go on to consider monounsaturated FFAs we have something like this:
MUFAs produce significantly less FADH2 so less reduction of the CoQ couple and are not used to generate nearly as much insulin resistance as fully saturated fatty acids. This is not surprising as MUFAs are desaturated versions of fully saturated fats and the desaturation process is largely activated by insulin. MUFAs can be thought of as a more carbohydrate tolerant version of saturated fats.
Of course by the time we get to linoleic acid there is even less FADH2 generated and we have very little ability to resist insulin when these are the main fatty acids being oxidised. Omega 6 PUFA facilitate the action of insulin but don't suppress it even when being metabolised in bulk:
So we can view a glucose system in balance with a fatty acid system where the input to the CoQ couple from the fatty acids controls insulin sensitivity to meter glucose access through manipulating insulin signalling or lack there-of.
Saturated fats suit low glucose availability, MUFA suit a mixed diet and PUFA are spawn of the devil. Near zero fatty acids in the mix rely on mtG3Pdh to regulate glycolysis flux.
I suppose we also ought to think of the situation under a large, uncontrolled fructose input through mtG3Pdh occurring at the same time as saturated fatty acids are being oxidised. That gives us this scenario:
Having two inputs reducing the CoQ couple (as well as a little input from SDH) is a perfect recipe for driving extreme reverse electron transport through complex I with the production of completely unreasonable quantities of superoxide and H2O2. This is the scenario of free radical mediated damage combined with serious insulin resistance. D12079B anyone? The problems are less severe with PUFA fats but this leaves us with a different set of problems, not for today. OK.
Before we go on to look at more human based scenarios using low fat diets I guess we need to consider insulin secretion by the pancreas. This is not solely controlled by glucose. In fact I think I’m going to include the only reference in this post as I don’t think I’ve cited this particular paper before, though I may have done so and forgotten!
Suppress most FFAs using nicotinic acid and you will completely abort the secretion of insulin generated by a glucose level of 12.5mmol/l. Replace the FFAs by infusion and you find that insulin secretion is markedly affected by the nature of the FFAs. The longer the acyl chain the more insulin is secreted. The more double bonds, the less insulin is secreted. At a FFA level around 0.1mmol/l, acutely induced, the pancreas will not secrete insulin in response to 12.5mmol/l of glucose. It seems to me that getting FFAs this low is well within the realms of possibility using a near zero fat diet. You are then in to the region of minimal insulin secretion combined with maximal insulin sensitivity. I know it’s a rat model, a perfused pancreas, assorted artificial lipid infusions, but the logic holds well. Insulin secretion and insulin response/resistance are remarkably similar processes.
So hypo insulinaemia with marked insulin sensitivity might well be the hallmarks of carbosis. I won’t reiterate my thoughts about hepatic insulin extraction except I see this as complementary to the reduced secretion under ultra low fat conditions.
As a True Believer I cannot see steady weight loss without reduced systemic insulin levels. Carbosis suggests that this is the real situation.
The phrase is ITIS, we all know what this stands for. Low enough fat can quite simply cripple the pancreas' ability to secrete insulin in response to glucose. Low enough fat and there is very limited ability to generate superoxide levels beyond normal PTP 1B inhibiting levels. If we accept that hyperinsulinaemia is the driving force of metabolic syndrome and all of its sequelae we have, under conditions of extreme fat restriction, the potential for reducing insulin while using a maximal carbohydrate diet. i.e. There is a health benefit to carbosis, possibly major, implausible as it seems.
There. I said it. You cannot argue with the physiology.
I believe this is what Denise Minger might be describing using "carbosis" as the corollary of ketosis. Under both of these conditions there is minimal insulin secretion but under carbosis there is enough insulin sensitivity working through mtG3Pdh to accurately regulate a near pure glucose metabolism. Fructose is no problem as there is plenty of "exchangeable" glucose for use in a substitution manner. Fatty acids have to be very low for "carbosis" to occur at all and it will be degraded far more easily by saturated fats than by PUFA, as per the ETC diagrams above and as per Denise’s examples.
The essential feature is low insulin. This is the commonality with ketosis. If there are going to be any health benefits of carbosis the low insulin will be the driving force.
So, am I a convert? This is not a religion, what I would ask is:
How effective is carbosis in the real world of T2 diabetes?
As Denise comments:
"More than half of those 100 diabetic ricers—63%—actually saw their fasting blood sugar drop by at least 20 mg/dL during the diet. Only 15% had their blood sugar go up significantly. The remaining 22 saw little to no change".
Translation: Blood glucose: 15% of people were f*cked. 22% it didn’t help. 63% could maintain carbosis.
Insulin usage:
"‘Twas a similar story in Insulin Land. Of the study’s participants, 68 entered the scene already dependent on insulin. As the carbs raged on, 21 of those insulin-injecters didn’t have to change their dosage; nine needed an increase (including four people who initially weren’t on any insulin at all); and—again comes the cruel, cruel defiance of prediction—42 slashed their usage significantly. In fact, 18 folks were able to discontinue their insulin entirely. Feasting on white rice. And sugar. And fruit juice".
Translation: Insulin usage: 13% were f*cked. 29% derived no benefit. 58% achieved carbosis.
How does this stack up against rather mild carbohydrate restriction in severe T2 diabetics?
This diagram says it all. It's from Haimoto et al in 2009.
All they did was drop carbohydrate intake to just over 130g/d. No ketosis. Look at the changes for the first 3 months in HbA1c:
No one needed to increase meds. No one failed to drop HbA1c. No one had to start on insulin. Most people dropped their sulpha drugs. The large spike upwards in the second section looks like one of the two drop outs. The other drop out seems to be lost in the variation in maintenance of control over the 3-6 month interval. Bear in mind that 130g/d is a VERY modest approach to low carbohydrate dieting in severe T2 diabetes. No ketosis, just 100% response rate to a modest carbohydrate reduction.
How can you compare carbosis with ketosis, or even mild carbohydrate restriction? It's like comparing boiled rice followed by boiled rice plus table sugar with a char-grilled fatty steak (rib eye is my preferred choice), buttered broccoli on the side plus Optimal ice-cream to follow. With extra double cream if you're losing too much weight.
The biochemistry of carbosis is very interesting. It might help just over a half of people who try it. Its therapeutic use seems to be of dubious relevance when real food can provide results in 100% of people who comply to carbohydrate reduction. It's strictly for the anhedonic out there but even these poor souls should be cautious about finding themselves in the group of 13-15% who end up f*cked, metabolically speaking.
No thanks.
Peter
Tuesday, October 06, 2015
Meet the researchers with the PKCζ deletion
Let's get this straight, right at the start: If you have cancer your outlook is probably worse if that cancer cell population has lost its ability to produce the metabolic regulator PKCζ. It's a bad news deletion.
We are looking at this paper (via David Ramsay, I think):
Control of Nutrient Stress-Induced Metabolic Reprogramming by PKCζ in Tumorigenesis
If you were remotely considering a ketogenic diet as a therapy for cancer management I think you might rightly be interested in the paper. Unfortunately it's quite technical (TL;DR perhaps Heather Buschman?) so perhaps it might be easier to go to the article in ScienceDaily for the take-home message. So initially let's look at the press release, the summary from which says this:
"Many scientists have tried killing tumors by taking away their favorite food, a sugar called glucose. Unfortunately, this treatment approach not only fails to work, it backfires--glucose-starved tumors get more aggressive. In a new study, researchers discovered that the protein PKCζ is responsible for this paradox. The research suggests that glucose depletion therapies might work, as long as the cancer cells produce PKCζ"
There are some pretty sweeping and unsupported statements here. If you actually read the paper itself you will find that there is a mass of information derived from cell culture under extreme (zero glucose, high glutamate) conditions which, while it does allow picking out the details of why PKCζ deletion might be so bad, tells you little about real life progression of cancer.
The group made two attempts to transfer their information from cell culture to something resembling real life. One approach was that they investigated, observationally, humans with colorectal cancer.
They found that in these people the outlook is worse if their particular cancer is PKCζ negative. Fair enough. However, attempted glucose restriction applied to humans with colorectal cancer is not exactly a widespread practice and was not mentioned in these patients. So it seems to be a reasonable assumption that those folks with PKCζ negative cancers are dying at an accelerated rate under glucose replete conditions, not under the conditions used in cell culture experiments. But we don't know for sure, there is no information about the blood chemistry or nutritional management of the patients.
The epic fail in the paper comes with the obligatory mouse model, tacked on near the end.
All you have to do is to mate cancer prone mice with mice which are PKCζ negative and a proportion of their offspring will be cancer prone and either PKCζ positive or negative. You can then test your hypothesis that glucose restriction promotes aggressive growth in PKCζ negative cancer prone mice, whose cancers will clearly be PKCζ negative too.
This should be easy.
Just feed the PKCζ negative mice something like that lovely F3666 ketogenic diet and compare them to those fed standard crapinabag. Obviously the low glucose levels from the ketogenic diet will promote early death in the PKCζ negative group as metabolism switches from glucose to glutamine and the cells develop an aggressive phenotype. The cell cultures say this will happen.
But they didn't do this. They actually fed D12079B vs crapinabag.
What is D12079B, you may ask, that you would use it to show that glucose restriction is Badness for PKCζ negative cancer victims?
D12079B is a typical Western Diet, sucrose/butter derived and is specifically marketed to produce metabolic syndrome in mice. Hyperglycaemia with hyperinsulinaemia. The exact, absolute, reliable opposite of the zero glucose used in all of the cell culture work.
Under glucose excess the animals with PKCζ knockout SHOULD have done at least as well as those on crapinabag, because all the cell culture work showed excess cancer growth during glucose RESTRICTION.
But this didn't happen. Under glucose excess the PKCζ knockouts died fastest of all the groups examined.
Let's just emphasise: At no point did the researchers attempt to limit glucose supply in anything even remotely resembling a live animal.
Does glucose restriction promote and aggressive cancer phenotype through a switch to glutamine metabolism, outside of cell culture?
No one knows. Certainly not the authors of the paper and don't get me started on the press release scribbler.
Personally I'm cautious about ketogenic diets in cancer. I'd expect them to do some good but only time will tell how much good and in which cancers.
But I can see a cop-out in a research paper a mile off. Did they try a few mice on F3666 and fail to report it because F3666 was protective? Or did they simply not dare test their hypothesis? At some stage there was a meeting of the senior researchers where the (extremely expensive) transition to a mouse model was discussed. They did not just stick a needle in a list of diets to choose D12079B. Years of work suggested looking at glucose restriction. They deliberately did the opposite. I shake my head in disbelief.
Peter
We are looking at this paper (via David Ramsay, I think):
Control of Nutrient Stress-Induced Metabolic Reprogramming by PKCζ in Tumorigenesis
If you were remotely considering a ketogenic diet as a therapy for cancer management I think you might rightly be interested in the paper. Unfortunately it's quite technical (TL;DR perhaps Heather Buschman?) so perhaps it might be easier to go to the article in ScienceDaily for the take-home message. So initially let's look at the press release, the summary from which says this:
"Many scientists have tried killing tumors by taking away their favorite food, a sugar called glucose. Unfortunately, this treatment approach not only fails to work, it backfires--glucose-starved tumors get more aggressive. In a new study, researchers discovered that the protein PKCζ is responsible for this paradox. The research suggests that glucose depletion therapies might work, as long as the cancer cells produce PKCζ"
There are some pretty sweeping and unsupported statements here. If you actually read the paper itself you will find that there is a mass of information derived from cell culture under extreme (zero glucose, high glutamate) conditions which, while it does allow picking out the details of why PKCζ deletion might be so bad, tells you little about real life progression of cancer.
The group made two attempts to transfer their information from cell culture to something resembling real life. One approach was that they investigated, observationally, humans with colorectal cancer.
They found that in these people the outlook is worse if their particular cancer is PKCζ negative. Fair enough. However, attempted glucose restriction applied to humans with colorectal cancer is not exactly a widespread practice and was not mentioned in these patients. So it seems to be a reasonable assumption that those folks with PKCζ negative cancers are dying at an accelerated rate under glucose replete conditions, not under the conditions used in cell culture experiments. But we don't know for sure, there is no information about the blood chemistry or nutritional management of the patients.
The epic fail in the paper comes with the obligatory mouse model, tacked on near the end.
All you have to do is to mate cancer prone mice with mice which are PKCζ negative and a proportion of their offspring will be cancer prone and either PKCζ positive or negative. You can then test your hypothesis that glucose restriction promotes aggressive growth in PKCζ negative cancer prone mice, whose cancers will clearly be PKCζ negative too.
This should be easy.
Just feed the PKCζ negative mice something like that lovely F3666 ketogenic diet and compare them to those fed standard crapinabag. Obviously the low glucose levels from the ketogenic diet will promote early death in the PKCζ negative group as metabolism switches from glucose to glutamine and the cells develop an aggressive phenotype. The cell cultures say this will happen.
But they didn't do this. They actually fed D12079B vs crapinabag.
What is D12079B, you may ask, that you would use it to show that glucose restriction is Badness for PKCζ negative cancer victims?
D12079B is a typical Western Diet, sucrose/butter derived and is specifically marketed to produce metabolic syndrome in mice. Hyperglycaemia with hyperinsulinaemia. The exact, absolute, reliable opposite of the zero glucose used in all of the cell culture work.
Under glucose excess the animals with PKCζ knockout SHOULD have done at least as well as those on crapinabag, because all the cell culture work showed excess cancer growth during glucose RESTRICTION.
But this didn't happen. Under glucose excess the PKCζ knockouts died fastest of all the groups examined.
Let's just emphasise: At no point did the researchers attempt to limit glucose supply in anything even remotely resembling a live animal.
Does glucose restriction promote and aggressive cancer phenotype through a switch to glutamine metabolism, outside of cell culture?
No one knows. Certainly not the authors of the paper and don't get me started on the press release scribbler.
Personally I'm cautious about ketogenic diets in cancer. I'd expect them to do some good but only time will tell how much good and in which cancers.
But I can see a cop-out in a research paper a mile off. Did they try a few mice on F3666 and fail to report it because F3666 was protective? Or did they simply not dare test their hypothesis? At some stage there was a meeting of the senior researchers where the (extremely expensive) transition to a mouse model was discussed. They did not just stick a needle in a list of diets to choose D12079B. Years of work suggested looking at glucose restriction. They deliberately did the opposite. I shake my head in disbelief.
Peter
Saturday, September 05, 2015
Protons (36) Glycolysis to lactate
Before we can even begin to think about metformin and mtG3Pdh we have to re examine lactate and glycolysis. It's difficult to over emphasise how interesting this hypothesis is:
Schurr, A. Lactate: the ultimate cerebral oxidative energy substrate?
I've no idea who Avital Schurr is. But he appears to be an anaesthetist, always a plus point, and he has a view of glycolysis which I really like.
I've blogged before on the astrocyte-neuron lactate shuttle and why I, from my own personal viewpoint, consider lactate to be the ideal mitochondrial fuel when reverse electron transport through complex I is best avoided. It behaves like glucose but without easy access to mtG3Pdh. With the exclusion of fatty acids from neurons the only reduction in the CoQ couple other than complex I then comes from complex II, part of the TCA. There is no input from ETFdh or mtG3Pdh. Pure acetyl-CoA, driving mostly through complex I.
The lactate shuttle is controversial.
Many years ago I recall a sketch on a comedy program, probably on Radio 4, where two politicians of irreconcilable views were invited in to the studio to debate the finer points of some policy by throwing half-bricks at each other.
I never really realised this at the time but the lactate shuttle polarises people. Lactate is viewed by many as an utterly useless, rather toxic end product of anaerobic glycolysis. It is a surrogate for hypoxia, hypoperfusion or mitochondrial failure. It is remarkably unacceptable to almost all physiologists that lactate can be a super fuel or even a fuel of any sort at all. Schurr goes through the arguments and the people and the papers and the logical fallacies and how two groups can look at the same data and draw radically differing conclusions. Think LCer vs vegan vs potato head. You look at the same studies but see different explanations......... And you know, we can't all be correct. Lactophobia is an emotional response. Schurr's words are ‘glucoseniks’ vs ‘lactatians’. You really have to read the paper!
The basic argument is that glycolysis always goes to lactate through pyruvate via cytoplasmic LDH 5. Whatever the oxygen availability. It's energetically favourable.
Lactate is then transfered to the mitochondria via a monocarboxylate transporter and fuels the TCA via pyruvate generated from the intra mitochondrial LDH, putatively LDH 1.
Partly this is redox related. Traditionally, using pyruvate:
Obviously, when you run out of NAD+ glycolysis would grind to a halt. But just look at how neat things become if you take glycolysis through to lactate:
Glycolysis, if it runs to lactate, is self sustaining. There is no deficit of NAD+, just an NAD+:NADH cycle. There is no need for the glycerol-3-phosphate shuttle, not for NAD+ regeneration anyway. Obviously, once lactate enters the mitochondrion it gets converted back to pyruvate with the generation of NADH. But this NADH is where it's needed, in the mitochondrial matrix, well away from the nucleus, ready to be processed by complex I.
How neat is that? Edward Edmonds suggested "elegant" as the descriptor. Yes, some hypotheses are so elegant the really have to be correct.
If it is correct you can then start asking questions about what mtG3Pdh is doing (if it's not regenerating NAD+) and how this might fit in with metformin. We're also back to what controls insulin sensitivity and how a cell regulates energy throughput. And fructose. And hyperglycaemia. Lots to think about.
Peter
Schurr, A. Lactate: the ultimate cerebral oxidative energy substrate?
I've no idea who Avital Schurr is. But he appears to be an anaesthetist, always a plus point, and he has a view of glycolysis which I really like.
I've blogged before on the astrocyte-neuron lactate shuttle and why I, from my own personal viewpoint, consider lactate to be the ideal mitochondrial fuel when reverse electron transport through complex I is best avoided. It behaves like glucose but without easy access to mtG3Pdh. With the exclusion of fatty acids from neurons the only reduction in the CoQ couple other than complex I then comes from complex II, part of the TCA. There is no input from ETFdh or mtG3Pdh. Pure acetyl-CoA, driving mostly through complex I.
The lactate shuttle is controversial.
Many years ago I recall a sketch on a comedy program, probably on Radio 4, where two politicians of irreconcilable views were invited in to the studio to debate the finer points of some policy by throwing half-bricks at each other.
I never really realised this at the time but the lactate shuttle polarises people. Lactate is viewed by many as an utterly useless, rather toxic end product of anaerobic glycolysis. It is a surrogate for hypoxia, hypoperfusion or mitochondrial failure. It is remarkably unacceptable to almost all physiologists that lactate can be a super fuel or even a fuel of any sort at all. Schurr goes through the arguments and the people and the papers and the logical fallacies and how two groups can look at the same data and draw radically differing conclusions. Think LCer vs vegan vs potato head. You look at the same studies but see different explanations......... And you know, we can't all be correct. Lactophobia is an emotional response. Schurr's words are ‘glucoseniks’ vs ‘lactatians’. You really have to read the paper!
The basic argument is that glycolysis always goes to lactate through pyruvate via cytoplasmic LDH 5. Whatever the oxygen availability. It's energetically favourable.
Lactate is then transfered to the mitochondria via a monocarboxylate transporter and fuels the TCA via pyruvate generated from the intra mitochondrial LDH, putatively LDH 1.
Partly this is redox related. Traditionally, using pyruvate:
- Glucose + 2 NAD+ + 2 ADP + 2 Pi → 2 Pyruvate + 2 NADH + 2 H+ + 2 ATP + 2 H2O
Obviously, when you run out of NAD+ glycolysis would grind to a halt. But just look at how neat things become if you take glycolysis through to lactate:
Glycolysis, if it runs to lactate, is self sustaining. There is no deficit of NAD+, just an NAD+:NADH cycle. There is no need for the glycerol-3-phosphate shuttle, not for NAD+ regeneration anyway. Obviously, once lactate enters the mitochondrion it gets converted back to pyruvate with the generation of NADH. But this NADH is where it's needed, in the mitochondrial matrix, well away from the nucleus, ready to be processed by complex I.
How neat is that? Edward Edmonds suggested "elegant" as the descriptor. Yes, some hypotheses are so elegant the really have to be correct.
If it is correct you can then start asking questions about what mtG3Pdh is doing (if it's not regenerating NAD+) and how this might fit in with metformin. We're also back to what controls insulin sensitivity and how a cell regulates energy throughput. And fructose. And hyperglycaemia. Lots to think about.
Peter
Monday, August 31, 2015
Confirmation bias is not just in my head
I've been sent a link to this study:
Body fat loss and compensatory mechanisms in response to different doses of aerobic exercise—a randomized controlled trial in overweight sedentary males
Bottom line: Moderate exercise produces equal weight loss to greater exercise. I'll come back to this later.
I commented in the last post that I consider leaving food on your plate is a very reasonable surrogate for experiencing reduced hunger. This shows up as weight loss. When we look at the converse, long term "accidental" weight gain, my perspective is the same. Eating an extra portion is a surrogate for responding to hunger. Long term hunger = Long term weight gain.
Let's say that again:
Fat people are fat because they are affected by hunger. Not gluttons. Not lazy. Hungry.
If people are going to lose weight on a long term basis they can only do this if they are not hungry. If they are not hungry they will reject food, establish an energy deficit and lose weight.
I may believe in CICO, but that CICO is controlled by hunger.
Back to the study. As the authors, struggling for a moment of lucidity, say:
"However, on the basis of the present findings, we propose that the introduction of a moderate dose of exercise may actually lead to an increase in NEAT without any increase in EI resulting in a “bonus effect,” whereas a higher dose of exercise may lead to an increase in EI and, thereby, a degree of compensation and less than expected loss of FM"
As clear as mud. Let's translate and simplify:
“… a moderate dose of exercise may actually lead to an increase in CALORIES OUT without any increase in HUNGER ... whereas a higher dose of exercise may lead to an increase in HUNGER [ie more eating] and … less than expected loss of fat mass”.
Exercise makes you hungry, certainly if you over-do it.
This is the authors' conclusion. I think they are correct. Other explanations are possible but they if miss the hunger component they are not of a great deal of help to anyone who wishes to understand obesity, even if they happen to be factually correct.
Peter
Body fat loss and compensatory mechanisms in response to different doses of aerobic exercise—a randomized controlled trial in overweight sedentary males
Bottom line: Moderate exercise produces equal weight loss to greater exercise. I'll come back to this later.
I commented in the last post that I consider leaving food on your plate is a very reasonable surrogate for experiencing reduced hunger. This shows up as weight loss. When we look at the converse, long term "accidental" weight gain, my perspective is the same. Eating an extra portion is a surrogate for responding to hunger. Long term hunger = Long term weight gain.
Let's say that again:
Fat people are fat because they are affected by hunger. Not gluttons. Not lazy. Hungry.
If people are going to lose weight on a long term basis they can only do this if they are not hungry. If they are not hungry they will reject food, establish an energy deficit and lose weight.
I may believe in CICO, but that CICO is controlled by hunger.
Back to the study. As the authors, struggling for a moment of lucidity, say:
"However, on the basis of the present findings, we propose that the introduction of a moderate dose of exercise may actually lead to an increase in NEAT without any increase in EI resulting in a “bonus effect,” whereas a higher dose of exercise may lead to an increase in EI and, thereby, a degree of compensation and less than expected loss of FM"
As clear as mud. Let's translate and simplify:
“… a moderate dose of exercise may actually lead to an increase in CALORIES OUT without any increase in HUNGER ... whereas a higher dose of exercise may lead to an increase in HUNGER [ie more eating] and … less than expected loss of fat mass”.
Exercise makes you hungry, certainly if you over-do it.
This is the authors' conclusion. I think they are correct. Other explanations are possible but they if miss the hunger component they are not of a great deal of help to anyone who wishes to understand obesity, even if they happen to be factually correct.
Peter
Sunday, August 30, 2015
Confirmation Bias in my head
Sometimes you get a reminder that you suffer from Confirmation Bias.
I do.
This morning I went back and dug out the study from Aberdeen:
Which carried the phrases:
"…participants were offered a fixed energy intake of 2000 kcal/d"
"In the isocaloric study, despite being served food of the same energy content, intake was slightly lower (66 kcal/d) and weight loss greater (7.2 ± 2.3 vs. 4.7 ± 1.0 kg in 4 wk, P less than 0.05), on the HF-LC diet after correction for unconsumed food"
"In the isocaloric study, despite being served food of the same energy content, intake was slightly lower (66 kcal/d) and weight loss greater (7.2 ± 2.3 vs. 4.7 ± 1.0 kg in 4 wk, P less than 0.05), on the HF-LC diet after correction for unconsumed food"
Feed overweight men 2000kcal/d of a mixed diet and they eat it all. Feed the same men 2000kcal/d of a mildly ketogenic diet (roughly ++ on ketostix) and they refuse to eat all of the food. What they reject gives a weight loss surfeit compared to when they were on the mixed diet.
There's no evidence they went to the gym on the quiet but the study protocol probably asked them not to do this. Assuming they have gyms in Aberdeen.
I don't give a monkey's about appetite score by VAS, lack of metabolic advantage in a study using 140g/d of carbs etc. Food left on plate = Not hungry.
How much simpler can it be?
This was triggered by an article linked to by Rose Nunez Smith via FaceAche which piqued my interest and which I read right through to the end. The article kept saying things which made sense and fitted with my view of reality. There was no author on the end so I went up to the top only to find it was Gary Taubes.
Well, it made me laugh.
It's good there are people writing for the NYT Sunday Review who point out what really matters. Bugger any metabolic ward study.
BTW re Aberdeen, with ketones at ++ it would have been interesting to know what the FFA levels were like but the arithmetic cited in the study suggests we didn't have a lot of UCP activity during this few weeks of ++ ketostix eating.
Peter
Tuesday, August 25, 2015
Starchy stable isotopes? I don't think so!
Have a read at this statement from Hardy et al 2015:
“…stable isotope analyses indicate a mainly carnivorous diet for Neanderthals; a wider range of isotopic values have been observed in contemporary Middle Pleistocene H. sapiens (Richards and Trinkaus 2009), indicating that considerable differences in the levels of starch consumption existed between these two species.”
Now, if you read this I think you might be led to believe that stable isotope analysis indicates that Neanderthals were carnivores and H sapiens ate a different amount of starch to a carnivore. I feel the implication of this sentence is that H sapiens ate "more-than-zero starch" during the Middle Pleistocene.
You would believe wrongly. Did you check the reference? No? Naughty. Richards and Trinkaus (2009) actually say this:
“As the method only measures protein intake, many low-protein foods that may have been important to the diet (i.e., high caloric foods like honey, underground storage organs, and essential mineral and vitamin rich plant foods) are simply invisible to this method.”
The data do not deny starchivory. But the data equally do not in any way support its occurrence. Starch, fruit and honey are invisible on stable isotope analysis. This is a gross mis-citation of Richards and Trinkaus by Hardy et al. Never believe stuff like this without checking the refs. Easy when it is a freebie in PLOS. What do Richards and Trinkaus actually say about diets of carnivorous Neanderthals vs H sapiens? Try this:
“There are now enough isotopic data to see patterns in the data, and they show that the Neanderthals and early modern humans had similar dietary adaptations, obtaining most of their dietary protein from animals, although some of the early modern humans obtained significant amounts of their protein from aquatic, and not just terrestrial, sources.”
You can tell H sapiens ate fish because aquatic food chains are long. The longer the food chain the greater the effect visible in stable nitrogen isotopes. They make fish eating carnivores look like hyper-carnivores. That's how they show up in the paper. Had humans eaten any significant amount of protein rich plants (hazel nuts get cited as a possibility) it would show a lower stable nitrogen ratio. There is no evidence for this.
Did early humans consume starch to grow their brain size? Stop laughing! No one knows, certainly to the point where a starchivorous paper has to mis-cite a completely non-supportive paper as being actually supportive of their rubbish hypothesis.
I love it.
Did you hear the one about Jennie Brand-Miller? Passthecream linked to this gem in the comments of the last post. Some things are just too funny not to share. Have a giggle. J B-M is second author on the starch-is-needed-to-grow-brains paper...
Peter
“…stable isotope analyses indicate a mainly carnivorous diet for Neanderthals; a wider range of isotopic values have been observed in contemporary Middle Pleistocene H. sapiens (Richards and Trinkaus 2009), indicating that considerable differences in the levels of starch consumption existed between these two species.”
Now, if you read this I think you might be led to believe that stable isotope analysis indicates that Neanderthals were carnivores and H sapiens ate a different amount of starch to a carnivore. I feel the implication of this sentence is that H sapiens ate "more-than-zero starch" during the Middle Pleistocene.
You would believe wrongly. Did you check the reference? No? Naughty. Richards and Trinkaus (2009) actually say this:
“As the method only measures protein intake, many low-protein foods that may have been important to the diet (i.e., high caloric foods like honey, underground storage organs, and essential mineral and vitamin rich plant foods) are simply invisible to this method.”
The data do not deny starchivory. But the data equally do not in any way support its occurrence. Starch, fruit and honey are invisible on stable isotope analysis. This is a gross mis-citation of Richards and Trinkaus by Hardy et al. Never believe stuff like this without checking the refs. Easy when it is a freebie in PLOS. What do Richards and Trinkaus actually say about diets of carnivorous Neanderthals vs H sapiens? Try this:
“There are now enough isotopic data to see patterns in the data, and they show that the Neanderthals and early modern humans had similar dietary adaptations, obtaining most of their dietary protein from animals, although some of the early modern humans obtained significant amounts of their protein from aquatic, and not just terrestrial, sources.”
You can tell H sapiens ate fish because aquatic food chains are long. The longer the food chain the greater the effect visible in stable nitrogen isotopes. They make fish eating carnivores look like hyper-carnivores. That's how they show up in the paper. Had humans eaten any significant amount of protein rich plants (hazel nuts get cited as a possibility) it would show a lower stable nitrogen ratio. There is no evidence for this.
Did early humans consume starch to grow their brain size? Stop laughing! No one knows, certainly to the point where a starchivorous paper has to mis-cite a completely non-supportive paper as being actually supportive of their rubbish hypothesis.
I love it.
Did you hear the one about Jennie Brand-Miller? Passthecream linked to this gem in the comments of the last post. Some things are just too funny not to share. Have a giggle. J B-M is second author on the starch-is-needed-to-grow-brains paper...
Peter
Monday, August 17, 2015
Sweden's dietitian advice? No thank you.
Hot off the press from Uppsala and Stockholm:
A high energy intake from dietary fat among middle-aged and older adults is associated with increased risk of malnutrition 10 years later.
"Contrary to what was expected, a high energy intake from total fat, saturated fat and monounsaturated fat among middle-aged and older adults increased the risk of exhibiting malnutrition 10 years later. However, this applied only to individuals with a BMI < 25 kg/m2 at the baseline. In conclusion, these findings suggest that preventive actions to counteract malnutrition in older adults should focus on limiting the intake of total fat in the diet by reducing consumption of food with a high content of saturated and monounsaturated fat."
Repeat after me. Association does not prove causation. How anyone dare suggest an experimental intervention on a large subpopulation of their nation based on an observational association within a subgroup of the target population is beyond me. How dare they?
It must be embarrassing to be a dietitian in Sweden nowadays but this sort of intervention recommendation is not going to decrease the stupidity index of mainstream dietary advice.
Hopefully sensible people will continue to ignore them!
Peter
A high energy intake from dietary fat among middle-aged and older adults is associated with increased risk of malnutrition 10 years later.
"Contrary to what was expected, a high energy intake from total fat, saturated fat and monounsaturated fat among middle-aged and older adults increased the risk of exhibiting malnutrition 10 years later. However, this applied only to individuals with a BMI < 25 kg/m2 at the baseline. In conclusion, these findings suggest that preventive actions to counteract malnutrition in older adults should focus on limiting the intake of total fat in the diet by reducing consumption of food with a high content of saturated and monounsaturated fat."
Repeat after me. Association does not prove causation. How anyone dare suggest an experimental intervention on a large subpopulation of their nation based on an observational association within a subgroup of the target population is beyond me. How dare they?
It must be embarrassing to be a dietitian in Sweden nowadays but this sort of intervention recommendation is not going to decrease the stupidity index of mainstream dietary advice.
Hopefully sensible people will continue to ignore them!
Peter
Subscribe to:
Comments (Atom)